Introduction
The public health rationale for management systems reform
Cambodia emerged from the period of civil conflict between 1975 and 1979 with a devastating loss of physical and human resources. Very few health personnel survived this period of turmoil. Since then the country has undergone a process of steady economic and social reconstruction. Although the population of 13 million lives predominantly in rural areas, rapid urbanization is occurring (Fig 1). However, high rates of illiteracy, infant and maternal mortality, communicable diseases, and lack of rural development continue to impede development progress.
Fig 1: Country map of the study area, Cambodia.
Following initial success with establishment of the Expanded Program of Immunization (EPI) in 1986, immunization coverage rates for children in Cambodia against the six EPI diseases (TB, DTP, polio, measles) have been static since 1995 (Fig 2). In 2002, 275 000 children under the age of 1 year were vaccinated against these six diseases1, primarily through health-centre outreach activities to villages in their catchment area, but a further 137 000 children under the age of 1 year were not fully vaccinated (33% of the target group).
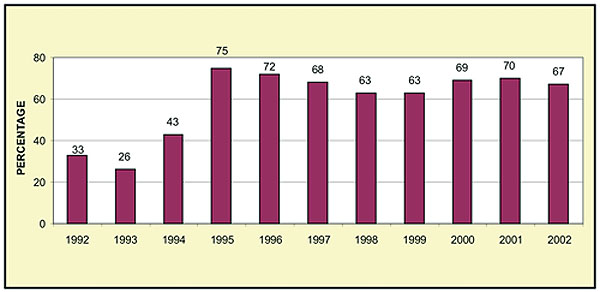
Fig 2: DPT3 Coverage rates, Cambodia 1992-2002.
Management reform background
Health system and policy: The health system has gradually developed a network of 970 health centers in 76 Operational Districts (OD) across the 24 Provinces of Cambodia. An OD is a health district that may consist of two or more political or administrative districts. An OD typically consists of a 100 000-population catchment area with a single secondary-level referral hospital. The primary level of care typically has a population catchment area of 10 000 with four to six health workers based at each health centre.
In 1994, the Royal Government of Cambodia (RGoC) proposed a health policy based on the reorganisation and decentralisation of health services, known as the 'Health Coverage Plan'2. Under this plan, implementation of health programs increasingly falls within the jurisdiction of District and Provincial Ministry of Health (MOH) officials rather than remain part of the pre-existing vertical management structure of the central MOH. Although some discreet vertical programs remain within the MOH, such as the National Immunization Program (NIP), the implementation of these vertical programs has been decentralized to Provincial health management.
In 2002, the Ministry of Health developed the Health Sector Strategic Plan 2003-2007, which focuses on six key areas (service delivery, human resource development, quality improvement, behavior change, health financing, and institutional development). Decentralization and de-concentration are identified as priority approaches within the key area of 'institutional development'3. The structure of the Cambodian health system is outlined (Fig 3).
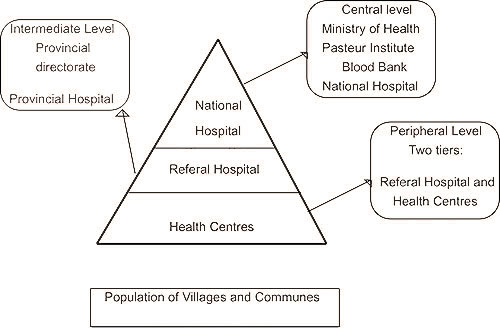
Fig 3: Structure of the Cambodian health system4.
Governance reforms
Following a period of civil conflict and a centrally governed economic structure, Cambodia is currently undergoing a steady transition towards a pluralist and decentralized model of governance. Decentralization is a cross-sectoral priority of the administrative reform agenda of the RGoC and is the focus of large-scale development assistance in areas rural development, health and education5. It is recognized that countries that have undergone a loss of centralised political or economic governance often experience post-reform declines in quality of public service provision. This has been the experience of countries in Eastern Europe and more recently of China6. The structural adjustment policies of the multilateral lending agencies have recently influenced other countries to embark on a process of devolution or decentralization that has been associated with a decline in quantity and quality of public services, particularly in rural and remote areas7-9. In response to changes in models of governance, a reorientation of national health program management is supported by a World Bank study of the impact of political decentralization on immunization coverage in 140 countries10. The study indicates that low-income countries can benefit from political decentralization, but cautions that a central program role remains essential in mitigating the potential negative effects of local government mobilization of health resources.
In recent years, Cambodia has researched and developed service delivery management structures based on a variety of contracting models. In the 'contracting out' model, loan funds were allocated to non-government organisations for management of district health programs. In the 'contracting in' model, contractors were assigned to co-manage district health services with existing government staff. In the 'comparison/control' model, existing district health services received budget supplements comparable to those available through 'contracting in'. These pilots have demonstrated important improvements in quality of service delivery and in health outcomes11-12. Both internal and external reviews found that after 3 years of implementation, the utilization of health services in the contracted districts improved significantly in comparison with the control districts13. However, other studies have highlighted sustainability and sovereignty issues associated with external contractors assuming responsibility for public services that are co-managed and funded by public authorities14.
Health system design is now reverting to a model of within-government contracting that is based on technical advice and assistance rather than on external control. This is consistent with the RGoC policy of decentralization and de-concentration, which seeks to locate accountability and co-management of public services through political channels (Provincial Governors and elected Commune Councils) and through administrative de-concentration approaches (financial delegations, sub-national planning systems). A human resource functional analysis has furthered the process of administrative reform, through research and consultation aimed at identifying the appropriate numbers and type of NIP staff, and by identifying pathways for de-concentration of program accountabilities to Provincial Health Departments (PHD)15. The availability of funds from the Global Alliance for Vaccines and Immunization (GAVI) for immunization service strengthening, and the emphasis by GAVI on a performance-based approach in the form of 'reward payments', has also motivated the NIP to develop innovative models of outputs-based agreements for sub-national levels of government.
It is within this health policy and research environment that the NIP has undertaken a program of management systems reform for the purpose of improved immunization coverage.
Aim
The aim of this article was to outline strategic responses undertaken by the NIP in support of improved immunization coverage and, where possible at an early stage, to identify lessons learned for future institutional responses to low coverage.
The process commenced with an analysis of the public health management situation in relation to immunization program performance. This was followed by an outline of the management reform steps to date, commencing with the integration of program planning with health sector planning and the introduction of coverage improvement planning and outreach services agreements. A central platform of this strategy has been the establishment of a system of outputs-based performance-based agreements between levels of government for improved immunization coverage. Finally, the NIP has developed and implemented a monitoring strategy in order to assess program performance and reform initiatives. (This summary is expanded in Results).
Methods
Sources of information
The following sources of information were used in preparing this report.
- NIP surveillance unit, which provided national immunization coverage information.
- A strategic planning exercise, undertaken by the NIP and international partners in early 2003 which included a problem analysis to identify key strengths and weaknesses in program performance.
- Microplanning exercises, undertaken by national planners, in partnership with Provincial, District and Health Centre staff, in 14 districts of Cambodia (more than 100 health centres). This involved an analysis of local area (health centre) immunization coverage including mapping, assessment of target populations, identification of numbers and locations of un-immunized children, identification of reasons for their un-immunized status, developing activities for reaching un-immunized children, and costing of proposed additional activities.
- A functional analysis of NIP human resources, conducted by the Human Resources Department of the Ministry of Health in partnership with WHO in 2002, which identified appropriate staffing numbers, location and type at central level.
- Government policy documentation.
- National and international literature.
The children's vaccine program at PATH, in collaboration with The University of Melbourne, appointed a management advisor and short-term human resource specialist in 2003 to assist the NIP to develop strategies for improved function and structure. This initiative focuses primarily on the development of a more efficient structure (integrated supervision), and enhancing the capacity of the NIP to de-concentrate functions to Provincial level. This is being undertaken through a process of consultation and group discussion with the senior management team of the NIP with advice from of other international partners (WHO and UNICEF) through a technical working group. Information gained from this process has been used within this article.
Data quality
Coverage data quality is assessed through several techniques. Data quality of the NIP has recently been assessed by GAVI evaluators and has demonstrated a 98% correlation between health centre statistics and national coverage data16. This assessment involved independent auditors randomly selecting four districts and tracking coverage data from health centre to national level. In addition, since 2002, immunization data from health centre and village level is validated via 'post activity assessment'. This involves national and Provincial immunization managers randomly selecting health centres and a village within the health centre catchment area and cross-checking data from interviews with all mothers of children more than 1 year old and pregnant women with the health centre register information. These assessments provide an additional opportunity to verify the register and document any 'errors' (ie incorrect vaccination, missed opportunities), and bring the information back to the health centre for debriefing and identification of corrective action. This system addresses the limitation of the data quality assessment in that it does not verify information down to village level and so is not always able to identify errors.
Results
Analysis of national immunization coverage data and identification of the response to falling coverage rates
During 2002, Cambodia experienced a fall in routine immunization coverage leading to increased pressure for improved performance. Additional pressure emanated from the recently instituted GAVI system of performance-based payments, determined by the attainment of national immunization projected coverage targets, and the National Poverty Reduction Strategy, which nominates DPT3 coverage as one of the 20 indicators for achievement of the 'millennium development goals'17. At the NIP planning18 workshop in June 2003, the paradox of spectacular immunization campaign success together with flagging routine immunization coverage was analyzed using a problem-solving approach. In contrast to 'static' routine immunization coverage rates, Cambodia, through campaign efforts, has eradicated polio and substantially reduced the reported incidence of measles from 13 827 cases in 1998 to 1361 cases in 20021. The strengths and weaknesses of both campaign and routine immunization which were identified during the workshop are summarised (Table 1). A clear lesson emerging from the strategic planning exercise was that the centralized and vertical nature of campaign efforts was a key ingredient in their success, along with high levels of guaranteed funding, and technical assistance and support for campaigns from partners.
Table 1: Analysis of National Immunization Program (NIP) performance (2002)18
In contrast, the routine immunization effort is led and resourced sub-nationally through the network of Provincial and District Health Departments, and health centers. The problem solving exercise identified the lack of clarity in roles and responsibilities between administrative levels, and weak central-level monitoring and supervision of sub-national levels. Additionally, the human resources functional analysis of the NIP recommended a further refocusing of NIP toward health sector integration and health system decentralization15.
Improved data reporting has also been suggested as a factor contributing to the reported fall in immunization coverage rates. A 2003 data quality audit reported a 98% consistency between health centre statistics and coverage rates reported at the national level16. This compares with an earlier independent audit in 2001, which reported a consistency rate of 87%. It is suggested that the weaknesses present in the system in 2001 may have led to artificially inflated coverage data which, when corrected, contributed in part to the fall in coverage levels in 2002.
In keeping with this assessment of the impact of decentralization and improved data reporting on apparent coverage rates, the NIP is highly aware of institutional constraints on performance relating to poor sub-national financing, human resources constraints at the primary level of care, lack of management support at middle levels (district and province), and the resource allocation tensions between centrally directed campaigns and sub-nationally planned immunization services.
In response to the issue of low coverage and the above identified constraints, and broader institutional developments in the areas of health sector and governance reform, the NIP has developed planning, organizational development and human resource responses to the problem of low coverage. These have included: integration of the NIP plan into the health sector plan; linking of health centre microplanning to District and Provincial health planning; establishment of a national monitoring and management support strategy; and instituting performance-based agreements between levels of government for improved immunization.
Each of these initiatives will be outlined.
Integration of the NIP plan into the health sector plan
Development of a sector-wide planning methodology: In 2003, the MOH developed a new planning methodology based on sector-wide 'key areas of work' and a more decentralized pattern of service planning based on objective setting at Health Centre, District and Provincial levels. The six key areas of work are: (i) service delivery, (ii) human resource development, (iii) institutional development, (iv) health financing, (v) quality improvement, and (vi) behavior change. Objectives set by the NIP and each health system level are linked to these six key areas. The other key feature of the new planning methodology is the development of costing tools for planners at each level, and the appropriate sequencing of planning procedures in order to match the budget cycles of the Ministries of Finance and Health.
The MoH Department of Planning facilitated the NIP planning meeting. The intent of this institutional co-operation is that sharing of common planning goals and processes will result in improved integration between national programs and Provincial and operational district health departments. The development of costing tools for program planners and a financial sustainability planning process has resulted in enhanced communication between the NIP and the MoH Finance Department. Similarly, the sharing of program planning goals and processes between the NIP and public health departments (as outlined in the new planning methodology) has the potential to integrate program planning into the system at sub-national levels.
Balancing technical and systems oriented planning objectives: Traditionally, the NIP Plan has been a vertical program (ie the NIP plan is not integrated within broader MCH activities but focuses solely on immunization activities19). Objectives have been essentially technical in nature, focusing on disease eradication, injection safety, vaccine wastage, and coverage improvement. Strategies focus on the introduction of technologies, vaccines and technical guidelines and so proposed innovations are primarily technical rather than systems oriented.
However, this reliance on vertical technical solutions for improved coverage is challenged by the persistence of low routine immunization coverage rates in the face of increased availability of technology, such as auto-disposable syringes, and readily available vaccines.
In 2003, the policy statement of the Ministry of Health emphasized sector-wide management, decentralization and de-concentration of financial planning and administrative functions within the health sector3. The identification of priority NIP activities for 2004 (Table 2) reflects a stronger balance in objective setting between technical and systematic responses to the problem of low coverage.
Table 2. New and priority activities of the National Immunization Program (NIP) 2004-2006
Initiation of needs-based microplanning processes
The NIP has instigated a process of Coverage Improvement Planning (CIP; Fig 4)20 with implementation funding support from GAVI, in order to accelerate progress towards national immunization coverage targets. The 'Reaching Every District'21 workshop conducted in Phnom Penh in 2003 provided some introductory tools for a coverage improvement strategy. The NIP adapted the tools and processes to the existing immunization circumstances in Cambodia.
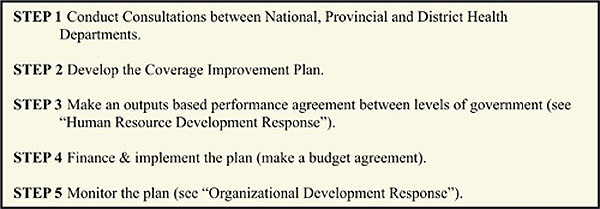
Fig 4: Process of Coverage Improvement Planning, Cambodia.
The aim of the Coverage Improvement Planning (CIP) process is to improve immunization coverage in Cambodia by developing and implementing immunization activity plans that are designed to reach additional children. The NIP commenced by selecting 14 priority districts based on a set of criteria that included numbers of un-immunized children, access to budget, and absence of international assistance.
Health workers and District and Provincial immunization managers identified a range of existing barriers to improved coverage, and developed plans which incorporated fully costed strategies to reach unimmunised children. Strategies included management support for health centres, communication (IEC) strategies, mini local-area 'campaigns', and 'extra' travel support for more distant locations. Activities funded under CIP were additional activities to reach additional unimmunised children and were thus complementary to standard health service delivery activities.
The three most important tasks in the microplanning process (CIP Step 3) were: (i) mapping the locations of missed children (ie the main areas for un-immunized children), (ii) analyzing the reasons why these are problem areas, and (iii) proposing solutions to reach these clusters of missed children.
This process of local area epidemiology demonstrated that the most significant reasons associated with the outcome of un-immunized status (in clusters of population) were social and economic in origin. These unimmunized populations included migrant workers, slum dwellers, ethnic minorities, traders, itinerant agricultural workers, fishing families, and those even further isolated by flooding, distance, insecurity and lack of knowledge (Case study, Fig 5).
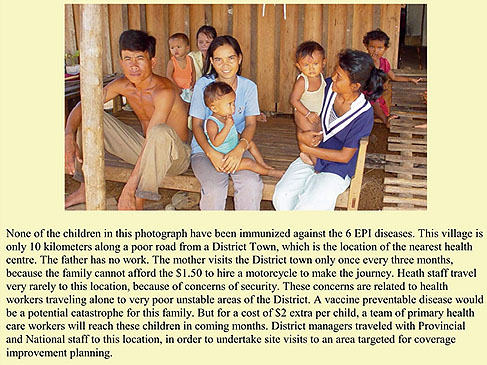
Fig 5: Case study: reaching the un-immunized children and families.
In an associated strategy, the NIP selected 10 districts for improved outreach services. These districts were selected on the basis of poor government disbursal of funds for outreach services. Performance-based agreements were signed between the district and national levels and were along the same lines as the CIP agreements. However, funding was restricted to support for health workers and for outreach travel, and logistic support (health worker per diem, transport and cold chain) and was not available for additional CIP activities.
Both strategies were reinforced by performance-based agreements and monitoring and management support.
Establishment of outputs-based performance agreements
Performance-based agreements for improved immunization were instituted which detail objectives, target populations, the budget agreement, and roles, responsibilities and duties of each system level (Table 3). The agreements are with the National-level and joint signatories include PHD and OD Health Managers (with EPI managers as co-signatories). The OD assume responsibility for instituting and monitoring sub-agreements with health centers in their respective catchment areas.
Table 3: Responsibilities for each system level in performance agreements for coverage improvement plans and outreach agreements
Of the funding, 70% is provided in advance, with a 30% final payment made on achievement of the coverage target, as verified by a post activity assessment (refer to Methods). At this time, it is too early to evaluate the impact of coverage improvement strategies on coverage rates. However, the early signs are positive. Of the 10 Districts that implemented the trial of the outreach agreements, eight have reached their targets in the first quarter of operation. After 5 months of operation in 2003, eight out of 10 CIP Districts are reporting annual coverage improvements for DPT3 that range from 3% to 31% when compared with the same period in 2002.
Establishment of a national monitoring and management support strategy
The development of CIP and performance-based agreements presented important management challenges for the NIP, such as how to monitor these agreements, and what role the NIP would play in supporting sub-national levels of government to reach coverage targets.
The functional analysis of the NIP management structure recommended multiskilling of managers and devolution of some tasks to mid-level managers. Further, the NIP Manager proposed a model of 'integrated national supervision' in order to increase management efficiency and accountability.
Based on these factors, a 'monitoring and management support strategy'22 (Fig 6) was developed (post-CIP and performance-based agreement introduction) with the stated purposes of:
- Supporting and advocating immunization coverage improvement and quality.
- Providing supportive management to middle level managers.
- Providing follow up corrective actions in support of coverage improvement and quality.
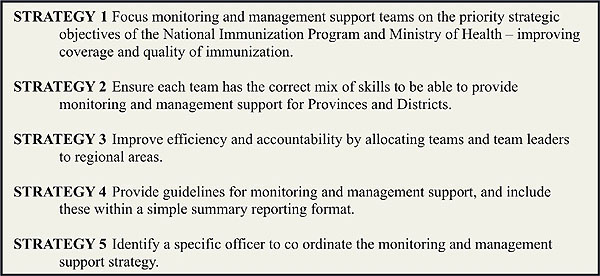
Fig 6: Summary of the monitoring and management support strategy.
Key elements of the strategy include multiskill composition of national monitoring teams, a regional (geographic) focus for management support (with the country divided into three regional multiskilled management teams rather than technical units operating nationally but within narrowly defined technical areas), and a focused objective of providing management support for Provinces and Districts to raise routine immunization coverage.
There are a number of risks associated with implementation including the potential under-skilling of teams in key technical areas and the risk of field information not being communicated into the NIP decision-making process. One of the most important approaches to managing the risks will be the development of an integrated management structure that is linked to the integrated monitoring process.
The NIP is currently developing an organizational development framework (both function and structure) that can accommodate the recommendations of the functional analysis and the requirement for strengthened and integrated management, particularly in the area of leadership, policy and planning, resource allocation, and monitoring and evaluation.
Historically, the emphasis in NIP planning has been on the attainment of technical objectives only. The current structure of the NIP reflects this with an emphasis on technical divisions and a less developed senior management structure that incorporates higher-level functions. The functional framework (Fig 7), developed with the assistance of a human resource specialist and currently under consideration by the NIP, is an illustration of the shift from an almost exclusive focus on operational technical functions towards development of central management functions of policy and national planning, leadership, financing and monitoring and evaluation.
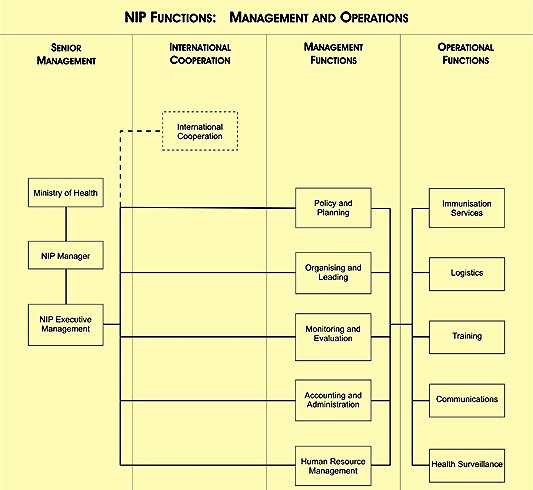
Fig 7: Draft functional statement of the National Immunization Program (NIP).
Discussion
Rationale - why management reform?
Questions have been raised as to the purpose of health sector reform and of institutional development in the context of improving immunization coverage. For example, why conduct functional analysis at all? Why reorganize into regions? What is the benefit of microplanning? Why do we need to contract instead of direct?
As with most public health endeavors, the primary motivation is reduction in population morbidity and mortality. Notwithstanding campaign success in the areas of polio eradication and the sharp reduction in the incidence of measles, immunization coverage rates in Cambodia have not risen, and have even declined since 1995. This is despite an extensive period of international collaboration and health infrastructure development. Additionally, an overarching process of political decentralization and administrative de-concentration is underway. Therefore institutional reform is essential to keep pace with economic and social change and to respond to the epidemiological setting of suboptimal coverage rates and persistently high child and maternal mortality rates.
The objective of institutional development is therefore to increase the capacity and optimize usage of public management in order to maximize population access to public services, and in doing so, impact positively on public health. This linking of proximal outcomes (health system developments), intermediate outcomes (health service access) and distal outcomes (health impact) is outlined (Fig 8).

Fig 8: Relationship between institutional development outcomes and public health impact.
In reference to the proximal indicator of system development, systems being introduced have included integration of the program and sector plans, introduction of CIP, establishment of performance-based agreements and the development of models of central program function and structure.
Additional institutional developments in this period have also included financial sustainability planning and development of a national communication strategy (not discussed here). Moreover, there are other forms of development such as new technology and new vaccine introduction that can impact positively on coverage. However, national and international experience indicates that institutional development, although not sufficient on its own, is nonetheless a necessary condition for coverage improvement, especially given the current pace of economic, social and political change in developing countries.
The role of integrated planning systems in strengthening decentralized health program management
Integration of immunization program planning with health system planning has the potential to improve coverage in several ways. A fundamental reason for the gaps in program performance between routine services and campaign efforts has been the fact that campaigns are centrally managed and routine services are not. With regard to campaigns, resources are mobilized centrally, directives are central, communications strategies are centrally driven (though sub-nationally assisted) and national political commitment is galvanized. In contrast, routine immunization services are essentially decentralized in their management, financing and planning. Service delivery is provided through the 970 health centers that are nearly exclusively rural. The finance for outreach services (through which 70-80% of children are vaccinated) is mobilized through Provincial treasuries and departments of finance and then de-concentrated to OD and NIP managers at OD level. Routine immunization performance is therefore far more heavily dependent on the effective function of the sub-national health system(s).
Integration of the immunization program with the broader health system through integrated health planning therefore provides the NIP with greater capacity to influence the resource allocation decisions of power brokers in sub-national agencies. In contrast, reliance on vertical planning exposes the immunization program to the risk of sole dependence on centrally managed international sources of finance, and distances EPI managers from the system management of Provincial and District Health Directors, who essentially are the main players in management of human and financial resources at the sub-national level.
Integration of vertical program planning with health system planning 'key areas of work' and processes is therefore a critical first step in aligning immunization with current and future health sector reforms. It places the NIP in a stronger leadership position to negotiate the potential benefits of decentralization and de-concentration, rather than being forced to respond in a delayed fashion to their potential risks.
The role of decentralized planning (microplanning) in promoting equity in health care provision
By identifying strategies, activities and finances to reach marginal populations, local area planning processes have demonstrated the capacity for local services to be pro-equity, pro-poor and pro-rights in relation to access to health. These form the three core values of MOH in Cambodia3.
Although the most prominent feature of the CIP process was the bringing of the health system into closer contact with remote and marginal populations, geographical distance and population dispersal remain major barriers to coverage improvement. Cambodia is a central plain area bordered by mountainous regions with dispersed, mobile and difficult to access populations, particularly in wet seasons. Flooding and poor roads often exacerbate the problem of geographical distance. The interaction of the exposures of sociological marginalization and geographic distance significantly increases the risk of un-immunized status. Across the country, the distance between health centers and villages varies from 35 km in the remote province of Mondulkiri to just over 1 km in the capital of Phnom Penh (Fig 9).
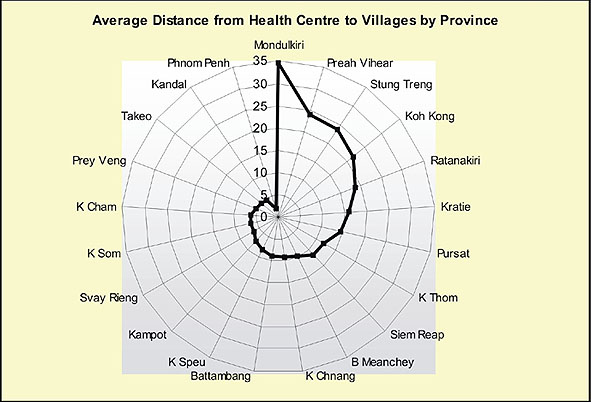
Fig 9: Average Distance from Villages to Health Centers by Province in Cambodia23.
There are more than 13 000 villages in Cambodia, and current MOH Outreach Policy24 dictates that each village should be reached once a month by health centre staff. It was recently estimated that annual outreach requires travel funding for 1.4 million km per year. This tests the financial sustainability of sole reliance on outreach as a strategy for reaching rural populations. The variation and distance within the social and physical landscape provides added impetus for a decentralized planning strategy that takes into account the real geographic distances and sociological conditions of marginal populations, in order that the most disadvantaged children can be reached by the health system.
Role of performance agreements in promoting sub-national accountability for health system performance
Cambodia is now experiencing the triple pressures of post-conflict, post-centrally governed systems, and multi-lateral lending pressure, and hence is highly exposed to the well-documented risks of hastily implemented policies of decentralization and de-concentration. This being the case, there are additional imperatives for Cambodia to adopt a model of administrative governance that links system levels in such a way as to help maintain system unity under the pressure of declining central governance. Contracting provides such an opportunity by providing both a chain of management and monitoring support that reaches to the grassroots level, and a chain of accountability that links back through the health system levels to NIP managers. This shift from 'central command' accountability to a de-concentrated style of governance has been evident in the character of consultations between national and Provincial levels prior to signing of the CIP Agreements. Whereas the tradition of vertical programs is to centrally direct, contracts are in contrast negotiated between joint signatories to the CIP agreements.
The international literature provides interesting case studies on the role of performance-based agreements and contracting in enhancing health system performance24,25. In Nicaragua, accountability of sub-national health authorities for service provision has been strengthened by stipulating responsibilities of service levels in the form of outputs-based performance agreements25. In the decentralized context of Burkina Faso, a World Bank study reported that the development of a system of outputs-based contracts for improved immunization coverage has resulted in improvements to some indicators26.
Cambodia has already experienced positive outcomes from trials of health system contracting. The system of program agreements outlined in this paper has demonstrated potentially significant benefits for improved coverage. Accountabilities for improved immunization are being de-concentrated to Provincial and District health directors and Health Centre Managers. As co-signatories to the agreements, primary accountability for coverage improvement shifts from the central to sub-national levels. This may be the key to shifting responsibility, and in turn, improving coverage, by motivating sub-national authorities to mobilize resources for achieving the health outcomes for which they can now be held accountable.
Strengthening management systems by building information linkages between micro- and macro-level planning processes
Perhaps the most interesting feature of the microplanning process has been the impact of local processes on national strategic thinking, particularly in the area of the national coverage improvement strategy. CIP has focused health planners on the clusters (numbers) of unimmunized in different locations and the reasons why these clusters exist. In a similar vein, numbers and locations can be applied to national area analysis of coverage rates.
The map in Fig 10 provides a snapshot of unimmunized children nationally.
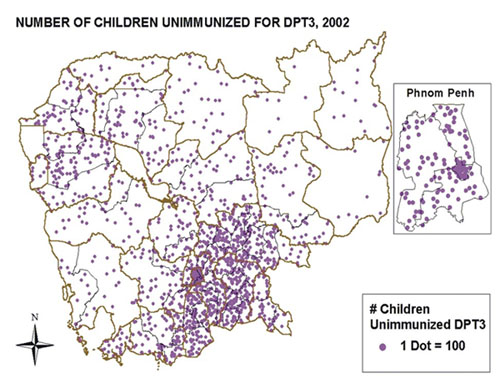
Fig 10: National Mapping of the Un-Immunized27,28.
Although the reasons for clustering of pockets of unimmunized at macro- and micro-level may vary (population density at the macro-level and social variables at the micro-level), microplanning has nevertheless reinforced a national epidemiological and needs-based approach to planning. That is, microplanning has resulted in a focus of management effort on development of performance-based strategies to target the highest numbers of unimmunized at both national and local level. This perspective has been further reinforced by the GAVI-funding system, which provides performance-based payments to developing countries based on the attainment of a mutually agreed number of children to be immunized.
In summary, both planning responses (sector strategic planning and health centre microplanning) provide important opportunities for the NIP to address the major reasons for plan failure - failure of resourcing for implementation and lack of match between organizational planning goals and community health needs25.
Establishing links between local health development and institutional development
A clear pathway can be observed between the various management reform processes of the NIP. The availability of GAVI funds to improve coverage in a flexible way encouraged the NIP to initiate microplanning processes. This in turn motivated the NIP to institute a system of performance-based contracts in order to promote accountability at the sub-national level for management of NIP funds. The establishment of the contract system stimulated the development of a monitoring and management support strategy in order to verify contractual outcomes and address non-attainment of results. Finally, the establishment of contracts and monitoring systems places pressures on managers to review structures in order to successfully and efficiently integrate field information into management decision-making. Management reform is hence a dynamic process, driven by system linkages established through needs-based planning, sector integration and contracting between levels of government (Fig 11).
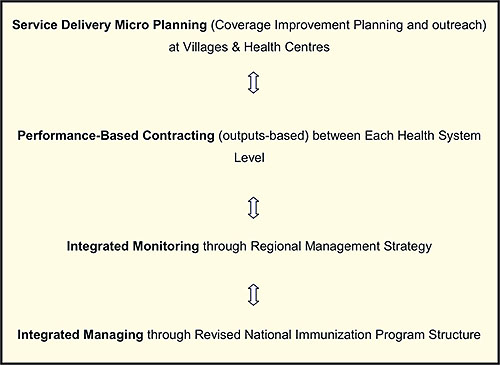
Fig 11: Linking of community health development to institutional development.
Conclusion
Immunization campaign successes in Cambodia have demonstrated that the application of appropriate management approaches in association with the secure financing for immunization can result in significant public health successes. However, new management approaches will be required to maintain and improve routine immunization coverage in a health system that is becoming increasingly decentralized. The NIP has recently undertaken management reform initiatives that have included integration of health sector and national program planning, strengthened micro-planning capacity, introduction of performance contracts and the establishment of an integrated monitoring strategy. In 2003, there are early signs that reform processes undertaken by the NIP have resulted in improved immunization coverage in targeted areas, and these should place the national program in a stronger position to lift immunization coverage in 2004.
An evaluation of the coverage impact of these institutional developments will be the subject of a later report. If coverage continues to improve in country-wide or selected locations, a more in-depth analysis will be required of the institutional correlates of improved immunization performance.
Acknowledgements
The senior management team of the NIP and the Ministry of Health Cambodia provided the leadership for these initiatives. The University of Melbourne in collaboration with the Children's Vaccine Program at PATH (funded through the Bill and Melinda Gates Foundation) provided technical assistance for these program developments in partnership with WHO and UNICEF. Dr Chea Kim Ly, Ms Ly Nareth and Dr Svay Sarath provided additional leadership direction in supporting these reforms. Andy Tucker provided advice on field implementation of contracting and CIP. Karl Jenkinson from the University of Melbourne undertook final editing of the manuscript.
References
1. Data Surveillance Unit. National Immunization Program. Phnom Penh: Ministry of Health, Royal Government of Cambodia, 2003.
2. Planning and Information Department. Health Coverage Plan. Phnom Penh Ministry of Health, Royal Government of Cambodia, 2002.
3. Cambodian Ministry of Health. Health Sector Strategic Plan 2003 - 2007. Phnom Penh: Ministry of Health, Royal Government of Cambodia, 2003.
4. Cambodian Ministry of Health. Ministry of Health Guidelines for Operational Districts Phnom Penh: Ministry of Health, Royal Government of Cambodia, 1997.
5. Ministry of Planning. Governance Action Plan. Phnom Penh: Ministry of Health, Royal Government of Cambodia, 2003.
6. Hesketh T, Zhu W. Health in China: The Health Care Market. BMJ 1997; 314: 1616-1618.
7. Duke T. Decline in child health in rural Papua New Guinea. BMJ 1999; 354: 1291-1294.
8. Collins C, Green A. Decentralization and primary health care: some negative implications in developing countries. International Journal of Health Services 1994; 24: 459-475.
9. Grundy J, Healy V, Gorgolon L, Sandig E. Overview of devolution of health services in the Philippines. Rural and Remote Health 3 (online) 2003: no 220. Available: http://rrh.org.au accessed 22 Dec 2003).
10. Khaleghian P. Decentralization and Public Services: The Case of Immunization. World Bank Policy Research Paper 2989. Washington DC: World Bank, 2003. Available: http://econ.worldbank.org/files/24757_wps2989.pdf (accessed 16 Dec 2003).
11. Asian Development Bank. Contracting Pilot Evaluation. Phnom Penh: MOH, 2001
12. Soeters R, Griffiths F. Improving government health services through contract management: a case from Cambodia. Health Policy and Planning 2003; 18: 74-83.
13. Bhushan I, Keller S, Schwartz B. Achieving the twin objectives of efficiency and equity: contracting health services in Cambodia. Manila: Asian Development Bank. Economics Research Department Policy Brief, Series 6 (online) 2002. Available: http://www.adb.org/Documents/EDRC/Policy_Briefs/PB006.pdf (accessed Dec 2003).
14. Kampong Cham Provincial Health Department, Hassall and Associates. Review of Performance Management Mechanisms. Phnom Penh: Ministry of Health, Royal Government of Cambodia, 2003.
15. National Immunization Program, World Health Organization. Functional Analysis of NIP Human Resources. Phnom Penh: Ministry of Health, Royal Government of Cambodia, 2003.
16. Global Alliance for Vaccines and Immunization. Draft Report on the Data Quality Audit Covering the Year 2002. Phnom Penh: Ministry of Health, Royal Government of Cambodia, September 2003.
17. Royal Government of Cambodia. Poverty Reduction Strategy 2004. Phnom Penh: Ministry of Planning, Royal Government of Cambodia, 2003.
18. National Immunization Program. Ministry of Health National Immunization Plan. Phnom Penh, Ministry of Health, Royal Government of Cambodia, 2003.
19. National Immunization Program. National Strategy on Immunization in Cambodia 2001 - 2005. Phnom Penh: Ministry of Health, Royal Government of Cambodia, 2003.
20. National Immunization Program. Introduction of Coverage Improvement Planning in Cambodia. Phnom Penh: Ministry of Health, Royal Government of Cambodia, 2003.
21. WHO Regional Office of Africa. Building capacity to reach every district with immunization services in the African Region: Status and perspectives. Vaccine Preventable Diseases Bulletin No. 033. (Online) March 2003. Available: http://www.afro.who.int/ddc/vpd/bulletins/2003/mar2003.pdf (accessed 17 Dec 2003).
22. National Immunization Program. Monitoring and Management Support Strategy. Phnom Penh: Ministry of Health, Royal Government of Cambodia, 2003.
23. Cambodian National Immunization Program. Financial Sustainability Plan. Phnom Penh: Ministry of Health, Royal Government of Cambodia, 2003.
24. Royal Government of Cambodia Ministry of Health. Outreach Policy. Phnom Penh: Ministry of Health, Royal Government of Cambodia, 2002.
25. Jack W. Contracting for health services: an evaluation of recent reforms in Nicaragua. Health Policy and Planning 2003; 18: 195-204.
26. Naimoli JF, Vaillancourt D, Kabore R, Balima Z. Partnerships within the public sector to achieve health objectives:Performance-based management in an evolving decentralized public health system in West Africa - The case of Burkina Faso. World Bank working paper 26947. (Online) 2003. Available: http://www-wds.worldbank.org/servlet/WDS_IBank_Servlet?pcont=details&eid=000160016_20031015171621 (accessed 17 December 2003).
27. National Immunization Program Surveillance Unit. National Map. Phnom Penh: Surveillance Unit, National Immunization Program, Ministry of Health, Royal Government of Cambodia, 2003.
28. Eager K, Garrett P, Lin V (Eds). Health Planning: Australian Perspectives. Sydney: Allen & Unwin, 2001.

