full article:
Context
Clusters and outbreaks of human parechoviruses (HPeVs) have become increasingly prevalent causing respiratory or gastrointestinal disease primarily in children aged less than 2 years1,2. Human parechovirus type 3 (HPeV3) is predominantly associated with sepsis and severe central nervous system infections; however, the gastrointestinal phenotype is rare3. The early consideration of parechovirus in infants presenting with undifferentiated abdominal illness atypical for sepsis or surgical cause may facilitate supportive management in some rural hospital contexts without need for transfer.
Our 318-bed rural hospital situated in Queensland, Australia has a joint adult and paediatric emergency department. The nearest tertiary paediatric intensive care unit is 384 km away. The child and adolescent unit of the rural hospital has 12 beds with care from general paediatricians, paediatric nurses and allied health professionals. The adult general surgical team provides care for paediatric patients in consultation with tertiary paediatric surgical teams.
We describe a rare presentation of parechovirus infection presenting as an acute abdomen and meningitis and its management in a rural centre. We aim to increase awareness of parechovirus in infants to medical professionals in rural areas.
Issues
A boy aged 11 days presented to the emergency department of an Australian rural hospital with fever, decreased oral intake and extreme irritability. He had no diarrhoea, or respiratory or urinary symptoms. He was born at term to a healthy mother by normal vaginal delivery. There were no maternal risk factors for sepsis in the baby and perinatal period was uneventful. He did not have any unwell family members at home.
On initial clinical examination in the emergency department, he had pale and mottled extremities with a rigid abdomen. The lower abdomen was noted to be erythematous with distension of the entire abdomen and severe irritability with palpation, suggestive of a surgical abdomen. Examinations of the heart and lungs were unremarkable. He was empirically treated with IV ampicillin, cefotaxime and metronidazole to cover gastrointestinal pathogens.
Diagnostic work-up with full blood count, urinalysis and blood cultures was normal (Table 1). Mild elevation of lactate was noted for venous blood gas, 3.1 mmol/L (reference value <1.0 mmol/L). There was mild derangement of the liver function tests with elevation of gamma-GT, 126 U/L (reference value 0–50 U/L); alanine transaminase, 61 U/L (reference value <51 U/L); and aspartate transaminase, 79 U/L (reference value <36 U/L). Cerebrospinal fluid showed a normal white cell count of 3 × 106/L (reference value for neonates 0–25 × 106/L) protein of 510 mg/L (reference value 200–1000 mg/L) and negative gram stain, culture and PCR for bacterial and viral pathogens.
Due to concerns about an acute abdomen, the local and paediatric surgical teams were consulted, and the case discussed with the paediatric intensive care unit team for potential transfer given the clinical condition. Ultrasound abdomen and upper gastrointestinal barium swallow were normal with no evidence of intestinal malrotation. Abdominal X-ray revealed no signs of necrotising enterocolitis (Fig1). As investigations for gastrointestinal pathology were unremarkable, the possibility of parechovirus was considered. Parechovirus PCR of cerebrospinal fluid was found to be positive.
Antibiotics were ceased following 36 hours of sterile blood cultures and confirmation of parechovirus infection. Supportive care provided in the rural hospital included IV fluids and insertion of a nasogastric tube given the possibility of surgical abdomen. The tube was removed after oral feeding was re-established. The patient was treated effectively in this rural hospital setting and did not require a transfer to a tertiary paediatric intensive care unit.
At his 2-months review in the general paediatric clinic, the patient had mild motor and neurological developmental delay with some increased tone in the lower limbs. At age 5 months, the neurodevelopment of the patient was normal. Follow-up at 21 months demonstrated largely typical development, with the exception of a mild delay in expressive language, for which early intervention by allied health specialists was initiated. The patient continues to have ongoing frequent developmental surveillance by a paediatrician along with neurodevelopment allied health specialists.
Table 1: Results of pertinent laboratory investigations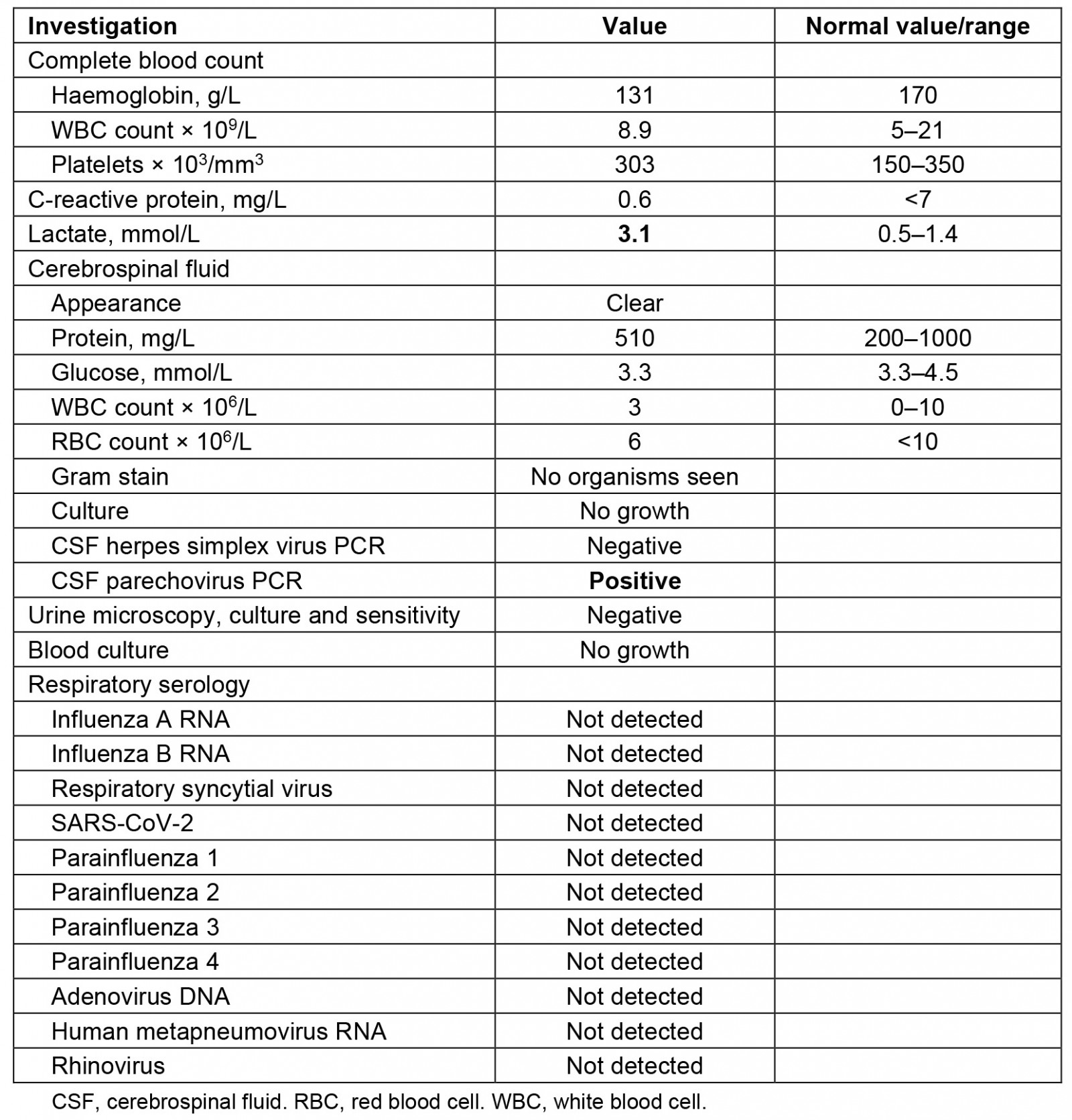
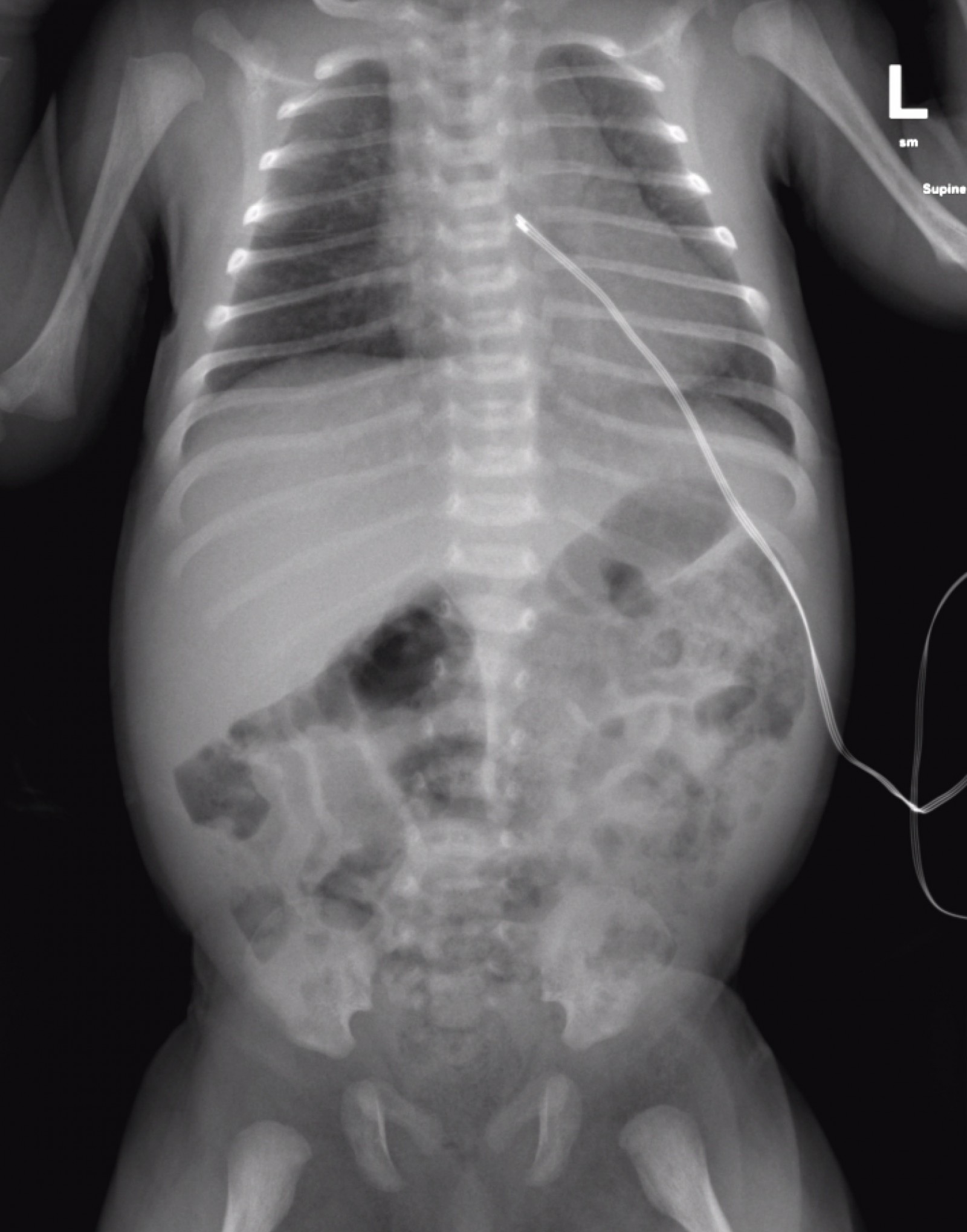 Figure 1: Abdominal plain radiography taken on admission. Mild faecal loading with no pneumatosis intestinalis or free intra-abdominal air.
Figure 1: Abdominal plain radiography taken on admission. Mild faecal loading with no pneumatosis intestinalis or free intra-abdominal air.
Ethics approval
The parent of the patient provided written informed consent for publication in a clinical case report.
Lessons learned
Human parechovirus infections in neonates and infants have been associated with several outbreaks throughout Australia, Northern Europe and the US, and have been linked with long-term neurological complications2-4. Symptoms of HPeV range from mild gastroenteritis or respiratory symptoms to severe systemic disease causing seizures or severe neurological damage3,5. HPeV3 has been recognised as an emerging cause of severe sepsis-like illness in infants aged less than 3 months3. Khatami et al documented the 2013 outbreak of HPeV3 in Australia, characterised by acute sepsis-like syndrome in infants2. The infants presented with high fever, tachycardia, poor perfusion and severe irritability, with 25% of neonates aged less than 2 months admitted to intensive care units2. HPeV3 has been linked to various complications including myocarditis in cases with extreme tachycardia and encephalitis, resulting in non-reversible changes on MRI2,4.
This case illustrates multisystem involvement of both meningitis and peritonitis associated with parechovirus infection. Previous case reports2,6,7 have described the unusual presentation of HPeV with severe abdominal distension. The mechanism underlying the development of peritonitis in parechovirus infections is not elucidated, but may be related to the virus’s ability to cause severe gastrointestinal inflammation, causing damage to the intestinal lining.
In this case, the symptoms of severe abdominal distension and tenderness led to the consideration of differential diagnoses such as Hirschsprung-associated enterocolitis, necrotising enterocolitis, volvulus and intussusception. Two previous patients with HPeV3 underwent exploratory laparotomies based on signs of acute abdomen. One of these infants underwent an exploratory laparotomy6, while the other infant had HPeV3 confirmed on PCR and a thickened, hyperaemic transverse colon consistent with necrotising enterocolitis8.
The pathogenesis of severe HPeV3 infection remains uncertain, although immune-mediated mechanisms similar to enterovirus have been hypothesised. This involves viral replication in multiple tissues, including the central nervous system and dysregulation of the host immune response4. It has been proposed that different receptor binding and increased neuropathogenicity of HPeV3 may account for its severe course compared to other strains of HPeV, particularly HPeV14.
The diagnosis of HPeV is made by viral culture or HPeV-specific reverse-transcriptase real-time PCR (RT-PCR) on CSF, blood or faecal samples. RT-PCR has been effective in detecting HPeV RNA rapidly within hours4. During the early stages of HPeV infection, viral RNA can be detected in cerebrospinal fluid and blood samples, while viral shedding in respiratory and faecal specimens persists for several days to weeks. Various studies found that HPeV causes meningoencephalitis with no pleocytosis in the cerebrospinal fluid and a significantly high protein level2,5.
In the present case, parechovirus PCR testing required a specific request to the microbiology lab as the cerebrospinal fluid samples were sent to the tertiary centre in Brisbane for analysis. Our rural hospital now has on-site access to the BioFire FilmArray Meningitis/Encephalitis Panel (Biomérieux; https://www.biomerieux.com/us/en/our-offer/clinical-products/biofire-meningitis-encephalitis-panel.html), which enables simultaneous detection of nucleic acids from multiple pathogens including bacteria (Escherichia coli K1, Haemophilus influenzae, Listeria monocytogenes, Neisseria meningitidis, Streptococcus agalactiae, Streptococcus pneumoniae), viruses (cytomegalovirus, enterovirus, herpes simplex virus types 1 and 2, human herpesvirus 6, human parechovirus, varicella zoster virus) and yeast (Cryptococcus neoformans/gattii).
HPeV testing should be considered for infants aged less than 2 months when it is clear that a surgical abdomen has been ruled out through examination and imaging. The early identification and consideration of parechovirus in the presentation of infantile septic-like abdominal illness is crucial in preventing unnecessary interventions. Hence with reassuring abdominal imaging studies, unnecessary intervention was avoided and the patient was suitably managed in a rural centre.
Studies have shown absence of correlation between detectable HPeV3 virus in cerebrospinal fluid and adverse long-term outcomes suggesting a lack of direct neuropathic activity of the virus1. MRI brain findings comparing HPeV encephalitis and hypoxic–ischaemic encephalopathy suggested that there may be vasculitis-mediated changes as opposed to direct cytopathic effects in the central nervous system1.
A study of Australian infants hospitalised for HPeV3 in 2013 found that 19% had significant concerns regarding their development 12–16 months after hospitalization5. In a minority of cases, HPeV can result in neurological sequelae such as cerebral palsy, learning disabilities, epilepsy and developmental abnormalities5. Complications of meningoencephalitis have been reported after severe HPeV infection with a distinctive pattern of white matter involvement with extension into subcortical white matter5. MRI best defines this periventricular white matter diffusion restriction5.
Severe symptoms of HPeV infections include acute flaccid paralysis, aseptic meningitis, neonatal sepsis and Reye syndrome4. Supportive management remains the mainstay of treatment for HPeV, as currently no effective antiviral therapies are available4,8. The early recognition and identification of HPeV infection in neonates presenting with abdominal sepsis and reassuring imaging has potential to reduce unnecessary and potentially harmful interventions. This can prevent unnecessary transfer to a tertiary centre, which may be a significant burden on families in rural regions9. Given the neurological complications of HPeV, neurodevelopmental follow-up is recommended until the infant reaches school age5.
Key points
- Early consideration of parechovirus PCR testing should be initiated in a neonate and in infants aged less than 2 months presenting with acute abdomen with no underlying cause on evaluation. This can prevent unnecessary interventions and be suitably managed in some rural centres with access to HPeV PCR testing and general paediatrician support.
- Management of parechovirus is limited to supportive care measures.
- Ongoing neurodevelopmental surveillance of patients with severe parechovirus meningitis is recommended.

