full article:
Introduction
Rural generalists provide holistic and complex medical care across the lifespan in rural and remote areas of Australia. They are uniquely placed within their communities to provide care in many settings, including in general practice and the emergency department of local hospitals1. In this context rural generalists are continually faced with making clinical decisions about whether patients can be managed locally, or if, and where, they need to be transferred.
Clinical reasoning is key to this process and can be divided into diagnostic reasoning and therapeutic reasoning. Diagnostic reasoning is concerned with information-gathering in order to form a differential diagnosis2. Therapeutic reasoning is concerned with the disposition and management of the patient, taking into account management options, context and likely therapeutic trajectory2.
The literature highlights the importance of context and complexity associated with clinical reasoning3. Diagnostic reasoning models such as John Murtagh’s safety diagnostic model (Box 1)4 support clinical learners by making unconscious cognitive processes more explicit, while for experts they provide a shared schema to review their decisions5. Much of the ongoing discourse focuses on the diagnostic reasoning process, and there are fewer studies relating to therapeutic reasoning, particularly as it relates to the rural and remote context6,7. Factors specific to the rural and remote context include the locally available resources, which can vary significantly between locations, and social factors, such as carer roles and travel distances8,9.
The aim of this study was to explore rural generalist therapeutic reasoning approaches in a simulated emergency scenario in the rural and remote context. The scenario was developed with the intent of focusing on patient management where there was uncertainty about therapeutic trajectory, prompting therapeutic decision-making.
The following research questions were addressed:
- What is the clinical reasoning process of rural generalists working in the hospital setting when managing patients with medical conditions, where it is unclear if they need escalation of care, including hospital admission or transfer?
- What are the contextual factors that are considered by rural generalists when making complex management decisions in the emergency setting?
- How are contextual factors considered by rural generalists when making their decisions?
The research team consisted of DP, LiW and JP, who currently practise as rural generalists with emergency medicine responsibilities. ED and AM are experienced registered nurses who develop, deliver and research healthcare simulations in their academic roles, and LuW is a rural academic clinician with experience in qualitative research.
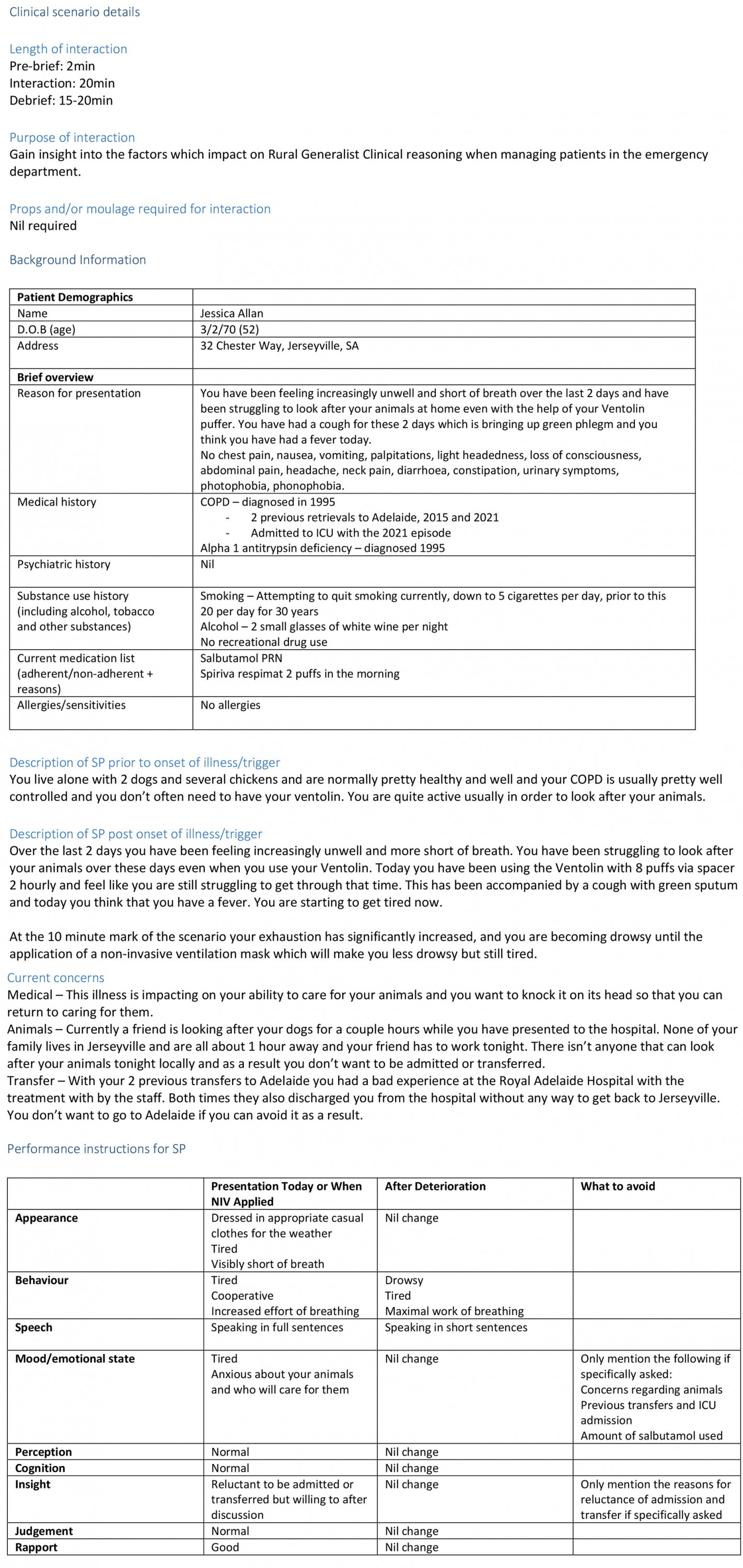
Box 1: John Murtagh’s Safety Diagnostic Model for general practice consultations4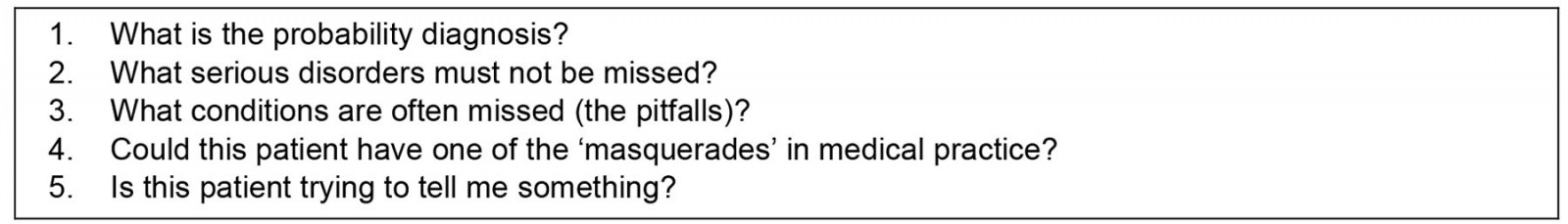
Methods
Study design
The study utilised an interpretivist epistemology, which recognises that individuals create subjective meanings based on their own experiences, and that discussion of meaning creates reality10. The research methods therefore sought to create a shared understanding of the world with interpretation shaped by the researchers’ own experiences of rural medicine11,12.
The research team developed a simulation scenario in the context of a small Australian rural hospital emergency department. The scenario was designed to prompt specific management decisions in participants. This enabled the researchers to explore rural generalist participants’ interpretation of clinical priorities, resource allocation and decision-making processes during a semi-structured interview.
Scenario
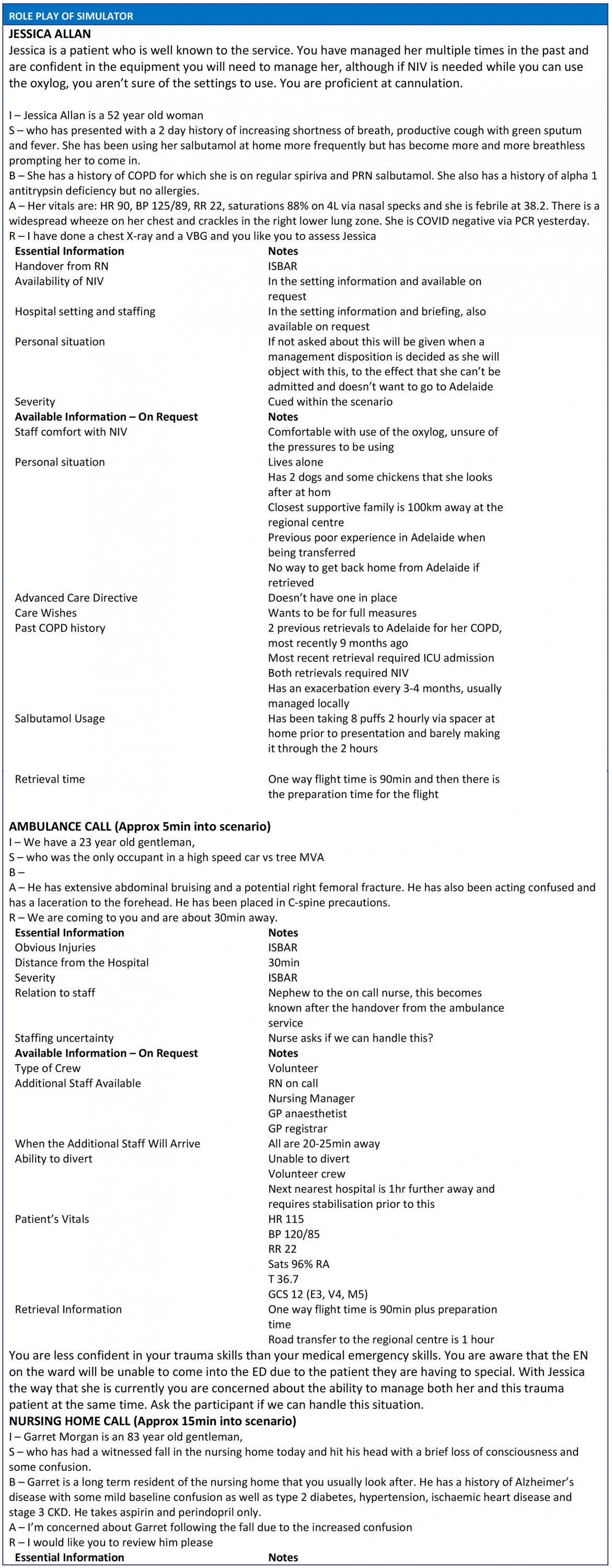
Development: The simulation was developed by considering content required to ensure participants understood the context of the health service and available clinical and human resources and, that presented patients in a manner that limited the complexity of clinical management yet maximised the need for observable behaviours and decision-making processes related to patient transfer and locations of care. An iterative process of scenario development was undertaken and involved expert consultation with simulation academics and rural generalists. The scenario was designed to ensure clinical accuracy, fidelity, representation of rural and remote context and simulation feasibility in a rural location. The final step in scenario development included rehearsal with experienced medical educators, the simulated patient, and the embedded participant registered nurse.
Health service context: During the simulation pre-brief, participants were provided with a written document describing the health service context, resources and availability of additional staff and retrieval services. The context was a 15-bed rural hospital with a two-bed emergency department, which serviced a population of approximately 1500. The nearest regional hospital was 100 km away, and a tertiary hospital accessible by aeromedical retrieval services was some 600 km away.
The participant was to commence their shift as the sole doctor. Their immediate team included one experienced registered nurse working in the emergency department. Additional staff included an enrolled nurse working in the ward of the hospital, a senior on-call registered nurse, and an on-call rural generalist with advanced skills in airway management and anaesthesia.
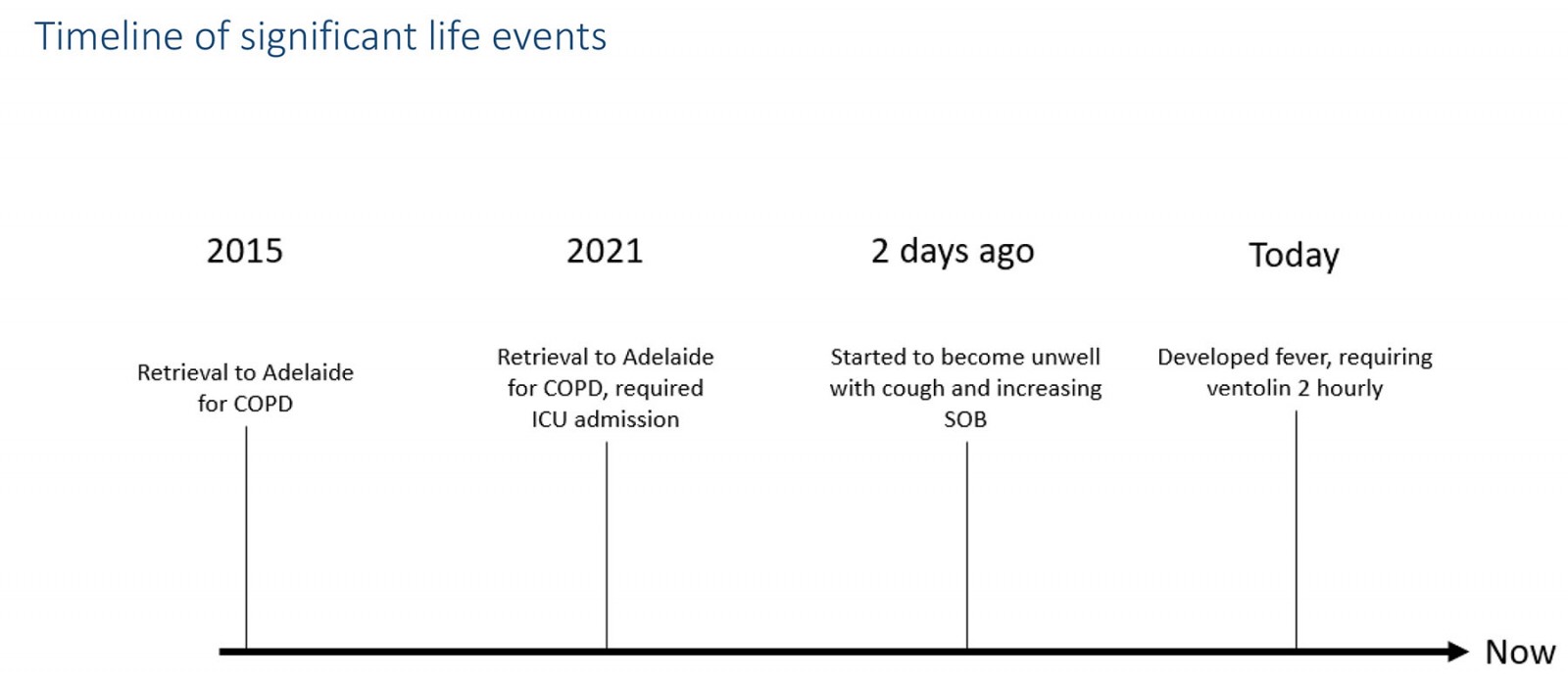
Decision triggers: The simulation scenario evolved over a 20-minute period. Complexities were interwoven through the clinical information provided, and the initial scenario involving a single patient evolved into a hypothetical multi-patient scenario at pre-determined intervals. The embedded registered nurse respectfully and assertively requested verbal directions/decisions from the participant. Clinical circumstances used to prompt decision-making included the primary simulated patient with complex social and clinical needs who was clinically deteriorating, an ambulance pre-alert of an incoming patient post high-speed motor vehicle accident, and an interrupting phone call from the local nursing home seeking permission to transfer a patient to the emergency department.
To represent the realities of rural practice, social and ethical complexities were embedded in the information provided to the participant. For example, the deteriorating patient was reluctant to be transferred due to past negative experiences in the tertiary hospital and the need to care for animals. The high-speed motor vehicle accident patient was the nephew of the senior registered nurse on call, and the nursing home patient had advanced dementia with ambiguity regarding an advanced directive.
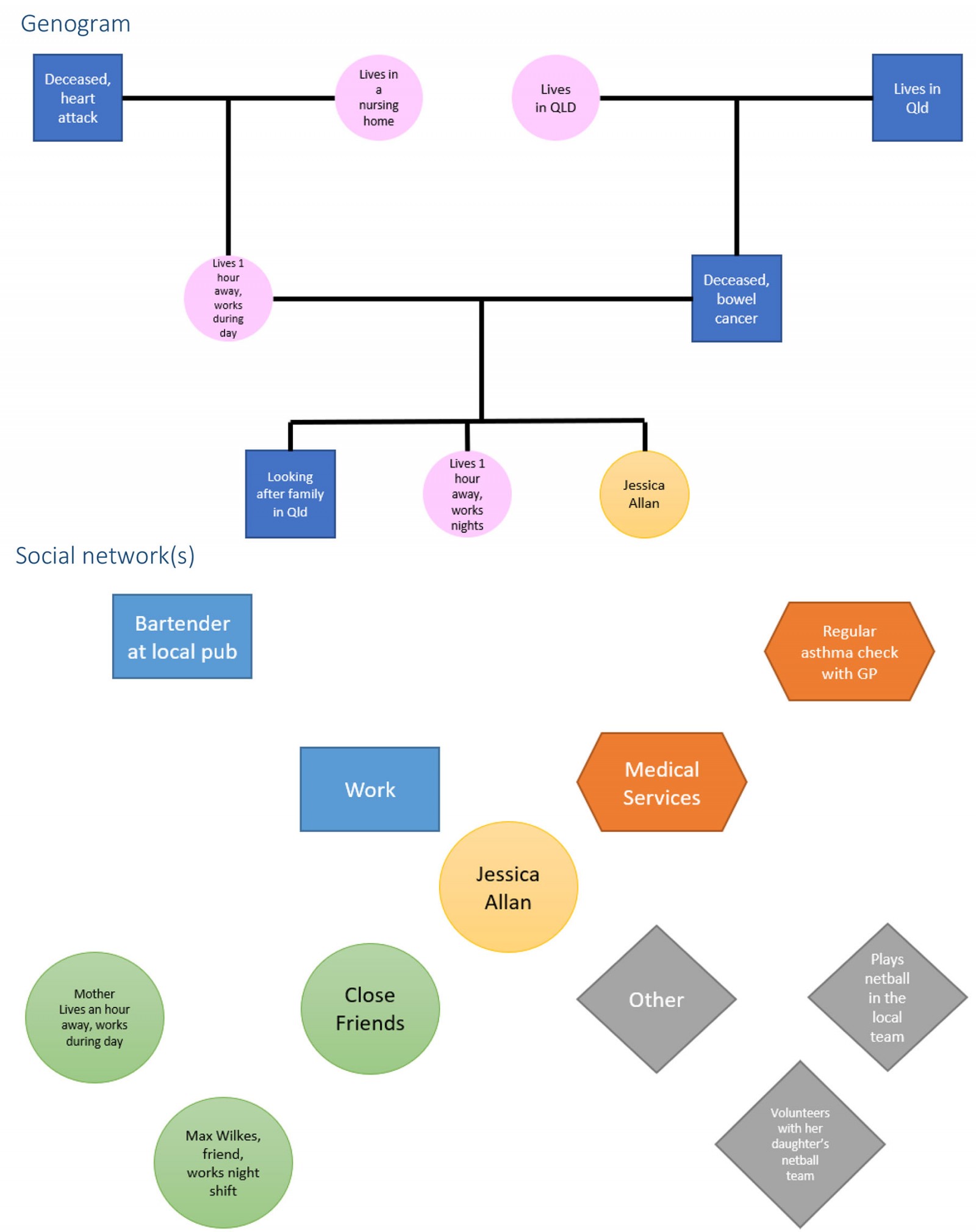
Further clinical details for the scenario are in Box 2. Further details of the fictitious rural town and simulation scenario are available in Supplementary materials 1, 2 and 3.
Box 2: Scenario clinical information
Participant recruitment
Rural generalists who were attending a conference hosted by the Adelaide Rural Clinical School for clinical supervisors were invited to participate in the research scenario. The research activity was advertised through direct email from the independent conference organiser prior to the conference and public announcements during the conference inviting rural generalists to a sign-up sheet. Individuals who signed up to participate in the research were consented by one of the research team members.
Interviews
Immediately following the scenario, the participants undertook individual semi-structured interviews to reflect on their therapeutic reasoning and the moments where decisions were considered. During the interview, participants were asked to discuss their reasoning and decisions for each of the patients in the scenario, with a particular focus on how the context impacted their decision-making; indicative questions are in Box 3. These interviews were recorded and transcribed for analysis and participants were given a chance to review their transcripts for comment and correction.
Box 3: Interview questions
Data analysis
An inductive content analysis approach was used with the assistance of NVivo v12 (https://lumivero.com/products/nvivo)13. Researchers reviewed the video of each participant’s scenario and read the corresponding interview transcript in full to develop a sense of the data. Open coding was undertaken by the lead researcher, supported by the research team, during six 2-hour sessions where the interview transcripts were read aloud to the group, and codes discussed and clarified.
This was followed by selective coding, with the contents of each code being reviewed by the lead researcher. During this review, codes were refined and redundancies removed. Codes were then arranged into nodes and categories. The content of categories was organised into themes to develop a mental model. The model was then tested through a review of the original scenario recordings by two members of the research team, who looked for evidence that the model could be applied to events that took place in real-time. Where there was agreement between the researchers, this was taken as supporting evidence for the mental model.
Ethics approval
Ethics approval was granted by The University of Adelaide Human Research Ethics Committee (Project number H-2022-091).
Results
Eight rural generalists undertook the scenario and interview over a 2-day period in mid-2022. The cohort was made up of four men and four women. Participants had a wide variety and length of experience working as rural generalists, varying from 1 year to more than 20 years. Of the cohort, seven undertook their medical degree within Australia. All participants had experience working in the emergency department of small rural hospitals in Australia, with seven having done so within the previous 12 months.
Throughout the simulated scenarios and interviews, participants described their reasoning approaches, which could be grouped into five broad themes: assessing clinician capacity to manage patient needs; availability of local physical resources and team members; considering options for help when local management was not enough; patient wishes and shared decisions; and anticipating requirements.
Assessing clinician capacity to manage patient needs
Participants discussed the importance of recognising their limitations in both skill and capacity. Participants recognised that these personal limitations were related to the simulated context and the risks of exceeding these limitations.
From the doctor’s point of view, I didn’t have the skill, obviously for things like intubation, so that skill itself needed a GP anaesthetist. (Participant 4)
Participants identified that their diagnostic reasoning process was a key component of assessing their skill set and capacity to provide immediate care. This initial step allowed for the assessment of patient needs, which consisted of a number of key factors, including patient disposition (risk factors, red flags and severity of illness), acknowledging uncertainty, likely therapeutic trajectory and optimal therapy. These factors were described without reference to context. For the second and third simulated patients in the scenario, participants acknowledged uncertainty of patient diagnosis or severity of injuries/illness, making inferences based on the limited information provided and anticipating initial and ongoing patient needs.
… a lot of red flags that worry me immediately, that we will need further assistance for. (Participant 6)
The importance of having a structured approach was also discussed by participants. This structure was reported to help focus the participants on the situation in front of them, and it minimised the risk of missing something critical. Participants referenced their real-world experiences, noting that they had refined this structured approach over the time they had spent working in their usual location, making it relevant to the simulated context.
Several participants emphasised that a factor for maximising resource impact involved ensuring the maintenance of situational awareness.
There’s this conflict between doing a lot of stuff, being too task focused and actually failing to see the bigger picture. And if you’re the only doctor in there, trying to manage two potentially quite sick patients. The worst you could do is actually go and … focus on a particular procedure and then you sort of, can’t see what else is happening. (Participant 3)
Available local physical resources and team members
Participants focused on what they were able to access locally for each patient in the scenario, with reference to their real-world capabilities. During the scenario participants sought to clarify what resources were available. During the interviews they discussed awareness of local resources as a factor critical to their reasoning process within the simulation. Featured in the discussion were not only the presence of equipment but also the resources not available locally and how these might be accessed.
The other thing is what your capacity in terms of equipment is. Where is your ceiling of care that you can provide to the patient. So here you can do an X-ray, you can do some informal bloods, you can do BiPAP [bilevel positive airway pressure] which is really helpful. But at the same time you sit there and go, I can’t do a lot more from here. (Participant 6)
Several participants contrasted the resources available within the scenario with those available in their usual setting, and discussed how their actions would have been different in the real world versus a simulated environment.
So if I was in [regional centre] I would probably hold onto [the initial patient], because I’ve got a physician and a HDU [high-dependency unit]. But if I was in [small rural hospital], probably would [transfer her], because, can I manage that patient overnight? Don’t know, depends on what else comes in. And it’s about making sure the patient’s safe. (Participant 8)
Participants also considered the available local staff and how to maximise the impact of the limited staff for the patients. Participants acknowledged that the situation was beyond the scope of the two-person team (the embedded nurse and themselves). Participants arranged for additional assistance from colleagues – both nursing and medical – to increase onsite skill set and staff.
Working as a team
Throughout the scenario participants sought information from the embedded nurse in relation to their skills and knowledge. Participants discussed the importance of having a good team around them.
[An] experienced registered nurse is worth their weight in gold, so always listen to what they're saying, they often have more experience than I might, in seeing patients like this, and may have seen things that have been done before that are useful. (Participant 2)
Participants noted the importance of opportunistic resources and staff, as well as local social knowledge, which could potentially unlock additional resources.
In a rural community, often your other staff are a really good resource, particularly long experienced RNs [registered nurses] who know the community, they might be related to half the community, or they know the social network for that person and so you can draw on them for advice and resources. (Participant 2)
Participants highlighted the importance of trust in other members of the team as a key factor. While reviewing the video scenarios the researchers were able to observe the building of trust between the participants and the confederate nurse (someone who is embedded within the simulation as a nurse). Participants described the importance of their assessment of the nurse’s competence in developing a clinical partnership.
Having a good RN [registered nurse] … he had a pretty good idea of where he wanted to go, as confident rural nurses will. And so you feel like you are more a partnership than you are actually being put on the spot. (Participant 7)
Participants also discussed the importance of getting the best out of other team members. This became more important as the number of staff available became more limited and was aided by communication within the team.
Because, you just have to work in tandem together. So that while I go, [the embedded nurse] can follow me. If there’s airway [problems], we get suction and we get the airway stuff. If there’s a pneumothorax we’re probably going to decompress it. (Participant 3)
The scenario design incorporated an issue frequently encountered in rural and remote health care: when the incoming trauma patient was known to be a relative of a staff member. For the scenario participants, this presented a challenge regarding getting the best out of this member of the team and balancing the immediate needs of the situation with the potential consequences.
I think this is going to be hard to do with one of us. And if I was the relative, I would want to have the best resources available to help my nephew, and even if I’m not involved if I can release someone else to be there… if she really doesn’t want to go in there, you aren’t going to make her go in there, and we’ll have to deal with it. So there’s going to be some consent there. But in a small community it is not unusual for family members to be the medical or nursing care. (Participant 7)
Safety of the team was considered more broadly by the participants.
If he’s got a head injury and combative it may actually be that he needs to be sedated and intubated for transfer because he’s not going to be safe for [the retrieval service] to transfer as he is. (Participant 2)
You don’t want to traumatise your staff, and, potentially have compromised care with emotion if they can’t step back from what is happening and just focus on the task they need to do. (Participant 1)
Considering options for help when local management was not enough
Participants acknowledged that patient care needs could change rapidly or escalate, and they discussed how this factored into their reasoning about possible transfer/retrieval. For example, all participants recognised potential for clinical deterioration in the initial patient and her needs after initiating CPAP. Participants considered the management options available to them locally and externally, through other services including retrieval and outlying hospitals. Access to these resources required knowledge and understanding of these external entities, and participants reflected on how this occurs in their real-world setting.
The retrieval service, tertiary centre and nearby regional centre were all identified as sources of additional support to manage acute events that, if resolved, could enable a patient to remain locally. Participants reflected on their real-world setting, with reference to the simulation.
So phoning a friend, [the retrieval service] are always fantastic, so getting advice from them, about the things that I could be doing locally before someone could come and support me ... Often it's a case of them saying, ‘Yeah, yeah, you're doing the right things.’ So it's just that reassurance, because for them, they do this stuff all the time (Participant 2)
Participants noted that the understanding of time to retrieval/transfer impacted on how early retrieval services would need to be activated, to ensure that they were available in a timely fashion. The reasoning for early discussion was to seek advice but also to allow the retrieval service to plan the utilisation of their resources. This early notification had to be balanced against the need to gather clinical information to provide the retrieval service with as much detail as possible to enable appropriate triage and planning.
In the grand scheme of things, when it takes them 2 hours to get here, waiting another 10 minutes to actually give them better information, so that [the retrieval service] … can prioritise appropriately. I don’t know what other calls they’ve got, so I need to give them the best information that I can. (Participant 7)
Participants recognised that while there are more resources at the regional centre than their own location, there is still a limit. Participants recognised that transfer to the regional centre may not be in the best interests of the patient.
The [regional centre] vs [the tertiary centre]. And what the risks and the pros and cons were, to decide on where we got [sent] her. Because if we transfer her to the [regional centre] and they weren’t able to cope with her and she wanted more, then we’ve wasted 6-12 hours, essentially where she could have deteriorated or [cardiac] arrested. (Participant 6)
With regards to the elderly nursing home patient in the scenario, a number of participants discussed that escalation of care may not have been appropriate. Participants described several factors in their reasoning process, including risk of distress, further patient deterioration, delays preventing timely definitive care and quality of life after the event.
It's not really appropriate to take somebody who is, or has dementia and say, ‘Hey, how about we send you off to a tertiary hospital, where they have a CT scanner, so you can have brain surgery,’ when your quality of life afterwards is going to be rubbish. (Participant 1)
Patient wishes and shared decisions
Participants engaged each patient in discussion of treatment options. This involved establishing the patient’s goals, determining their competency to consent, ensuring their understanding of the situation, and shared decision-making.
Participants referred to their frequent real-world experience with patients who had a strong desire to remain within the community instead of leaving town to receive care.
A lot of people just sit there and say I do not want to go to [the tertiary centre]. There’s probably a few who just don’t want to go to town, and then there’s often various experiences further from that, in terms of going to major hospitals, and being with people who don’t know them … So everyone’s often very happy to come back into the [local] hospital which is extremely small, like the scenario. (Participant 6)
Patient competence also featured in the interview responses. Participants acknowledged that competence of the simulated patient with respiratory failure could be impaired by her condition. Participants reflected on this and considered the course of action they may have taken.
But also, [she is] actually getting hypoxic, so that’s going to impede your judgement as well. If she became unconscious … I’d be saying, ‘No, we are doing everything we can here,’ because we haven’t … Because we really haven’t got her giving informed consent. (Participant 5)
Participants also referenced the importance of the patient’s understanding when discussing the available options. Part of this included setting realistic expectations with the patient and family or managing these expectations.
If you get better before retrieval, you won’t have to go. But we just need to bear in mind that’s an option if you don’t get better here. And look, at the end of the day, they need to be in the right place for care. (Participant 7)
Anticipating requirements
Participants discussed how they managed the multiple patients within the scenario. They reported the need to re-triage as new information became available and new patients were added to the scenario. They described this as a typical part of the role of running a rural or remote emergency department, even when critical emergency situations are not occurring.
The majority of the time as an on-call GP in a rural hospital, you’re prioritising and triaging but it's not with emergencies, you know it’s a bit different. You know, footy injuries or laceration or chest pains, but nobody who's actually critically unwell. But you still use that whole principle of prioritising things, and so you’re still practicing it every day. (Participant 2)
When considering which resources were needed and the resource capacity for managing a patient, participants considered not only what was needed at the time, but also considered what would be needed in the future. This consideration of future health service capacity played a significant role in decisions regarding the location of management.
They need to be in the right place of care. And it could be you’ve got a nurse out who’s on 24 hour cover in a small country town of 300 people. They can look after them but they can’t continue to look after them, so therefore we need to retrieve them … It’s not that the nurse is incapable of managing the case, it’s just that they can’t do it indefinitely. (Participant 7)
When patients were added to the simulation, participants discussed the importance of judicious resource use. In particular, they explored appropriate resource allocation between patients, the goal of which appeared to be to achieve an optimal outcome for the maximum number of patients within the resource constraints. This was exemplified when a participant was considering an invasive procedure but decided against it based on resource capacity.
I need to know whether my nursing staff are comfortable with managing … more complex equipment. We put in an art [arterial] line or a central line, it’s easy for you to put one [in], but who’s going to look after it? (Participant 3)
Therapeutic reasoning model
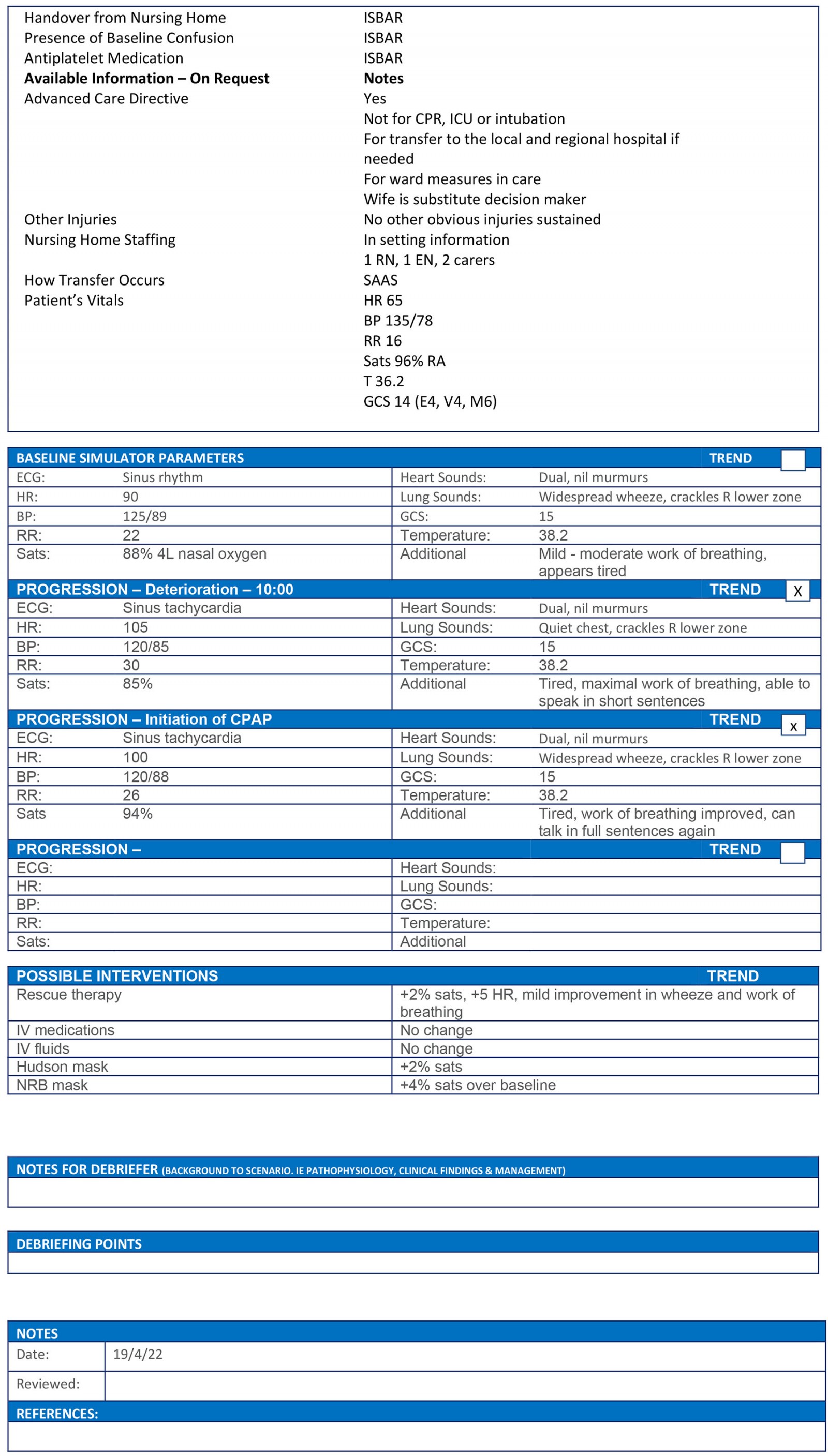
Following analysis of interviews, we developed a mental model comprising seven cognitive prompts that described the process of therapeutic reasoning by rural generalist participants.
- ‘What can I do for this patient locally and what are my limits?’
- ‘Who is on my team and who can I rely on?’
- ‘What are the advantages and disadvantages of local management vs transfer?’
- ‘Who else needs to be involved and what are their limits?’
- ‘How can we align the patient’s wants with their needs?’
- ‘How do we adapt to the current and future situation?’
- ‘How do I preserve the capacity of the health service to provide care?’
Upon review of each simulation recording, considerable evidence was found to support the mental model. There was evidence that all prompts (except one) were considered by the majority of participants in real time. The prompt ‘How do I preserve the capacity of the health service to provide care’ appeared to be considered by half of the participants during real-time evolution of the scenario.
Discussion
This study explored the therapeutic reasoning processes of rural generalists using a simulated multi-patient emergency scenario. In making management decisions for patients, study participants described multiple factors they considered, which were grouped into five main themes: assessing clinician capacity to manage patient needs; availability of local physical resources and team members; considering options for help when local management was not enough; patient wishes and shared decisions; and anticipating requirements. With these themes we developed a mental model using cognitive prompts that described the therapeutic reasoning process (outlined in Table 1), which we have called the Pellegrini Therapeutic Reasoning Model. The model may be a useful framework to facilitate case discussion among clinical learners. The model is also the first to describe the explicit cognitive processes occurring that underpin therapeutic reasoning of doctors working in rural and remote Australia. Figure 1 shows the relationships between the components of the mental model.
Participant interviews demonstrated that agility of decision-making was key in a situation that was intrinsically uncertain. In determining optimal location of care, participants described balancing needs of the patient with their own capabilities, the local resources available and likely therapeutic trajectory. In exploring clinical reasoning in other contexts, Preisz14 describes the conundrum of fast versus slow thinking and the benefit of ethical reasoning – that is, considering patient and social issues beyond the bounds of traditional diagnostic reasoning. Similarly, Higgs argues that contextual experience is key in these types of situations – so-called ecological decision making, where doctors draw on practical wisdom embedded in ethicality, reflexivity and deeply embodied accepted custom5. The term ‘ecological’ reflects the interdependence of decision-making parties (in this case the rural generalist, local team members, the patient, distant referral centre and the retrieval team members), and the constant need for networking between these groups5. It was therefore illuminating that participants often referenced their real-world experience in order to be able to better deal with the circumstances of the simulation.
Staffing and physical resources were one of the key factors discussed by participants during their interviews. In 2021, Kerr et al sought to create a system to simply communicate the resources available in any Australian emergency department and identified that there was wide variation in staffing and equipment15. Baker et al confirmed this variation in a 2022 study and found that this had led individual departments to adapt the ways in which they provided care to patients, with the goal being to maximise patient outcomes in a sustainable manner16. Participants frequently made reference to the resource difference in the simulation to their real-world setting during their interviews and would discuss the impact of this on their therapeutic reasoning.
Transfer of the patient to the regional or tertiary centre was considered by all participants as an appropriate step for patients who needed a level of care that was not available locally. While exploring the impacts of interhospital transfers, Feazel et al emphasised the potential benefits of patient transfer to patient outcomes17. The authors also noted that interhospital transfer was not an unalloyed benefit, with risks of delays, deterioration during transfer and the possibility of neglecting patient wishes17. In 2019, BehaviourWorks Australia produced a report in an attempt to improve transfers within Victoria. In this report they acknowledged several constraints that can impact upon patient transfer18. These factors included the resource capacity of the receiving hospital service and that of the transfer services themselves18. In our study, participants acknowledged the potential risks versus benefits of patient transfer, and this was incorporated into their therapeutic reasoning approach, particularly with respect to the management of critically unwell patients.
Cognitive prompts can be used to explore the decisions of the experienced clinician through a reflective and critical lens. This explicit approach to describing clinical reasoning overcomes problems with explaining ‘fast thinking’ to clinical learners as described by Preisz14. The foundation for fast thinking is experience and heuristics that are developed over time6, so developing mental models should be a key step in our approach to teaching clinical reasoning. In our study we developed a mental model using cognitive prompts, for which we found ample evidence in real-time playbacks of scenarios. Our model could be adapted to teach clinical learners or utilised in future research studies examining decision-making in other rural and remote healthcare contexts, including in simulation and real-world environments.
Table 1: Pellegrini Therapeutic Reasoning Model – components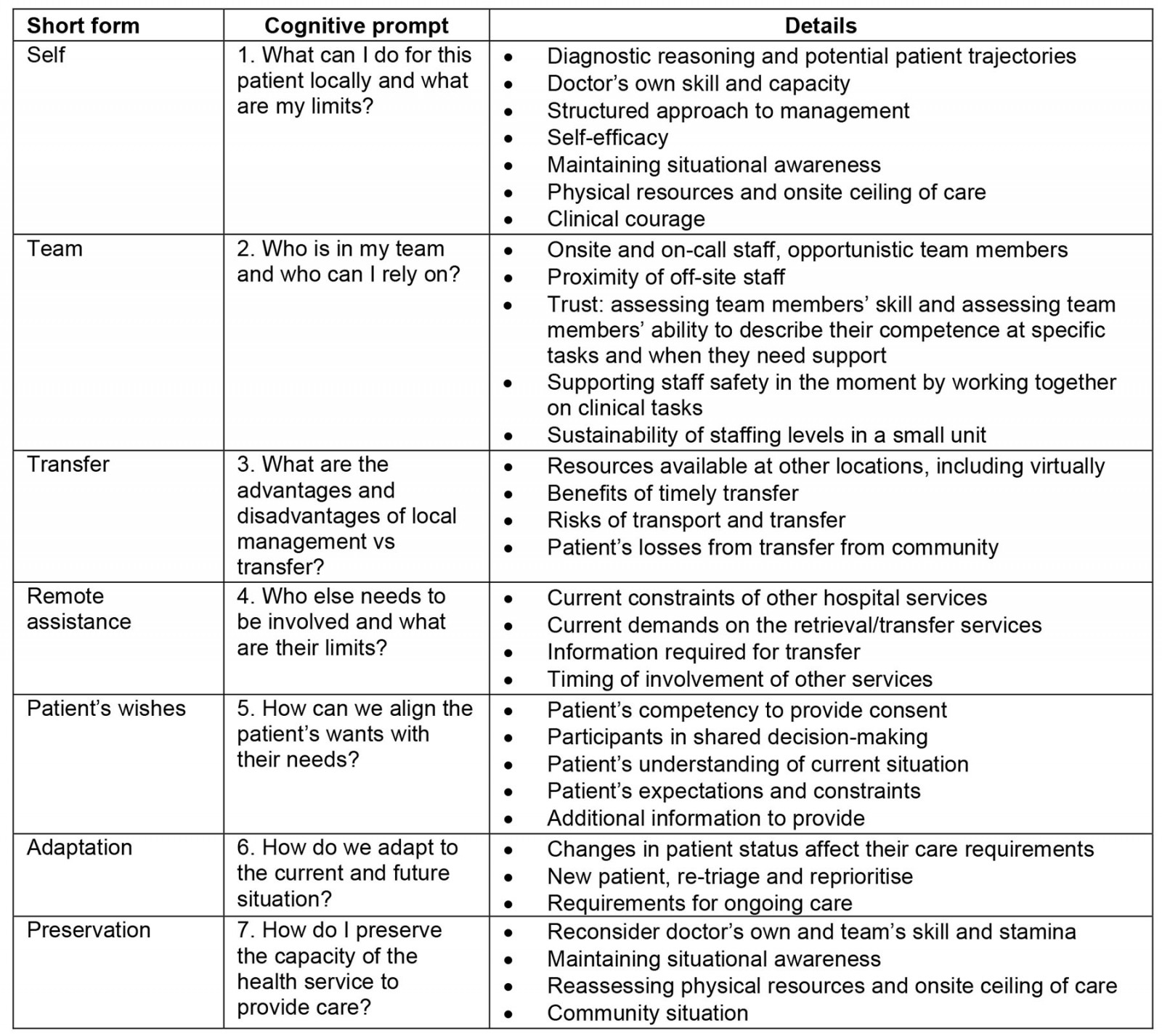
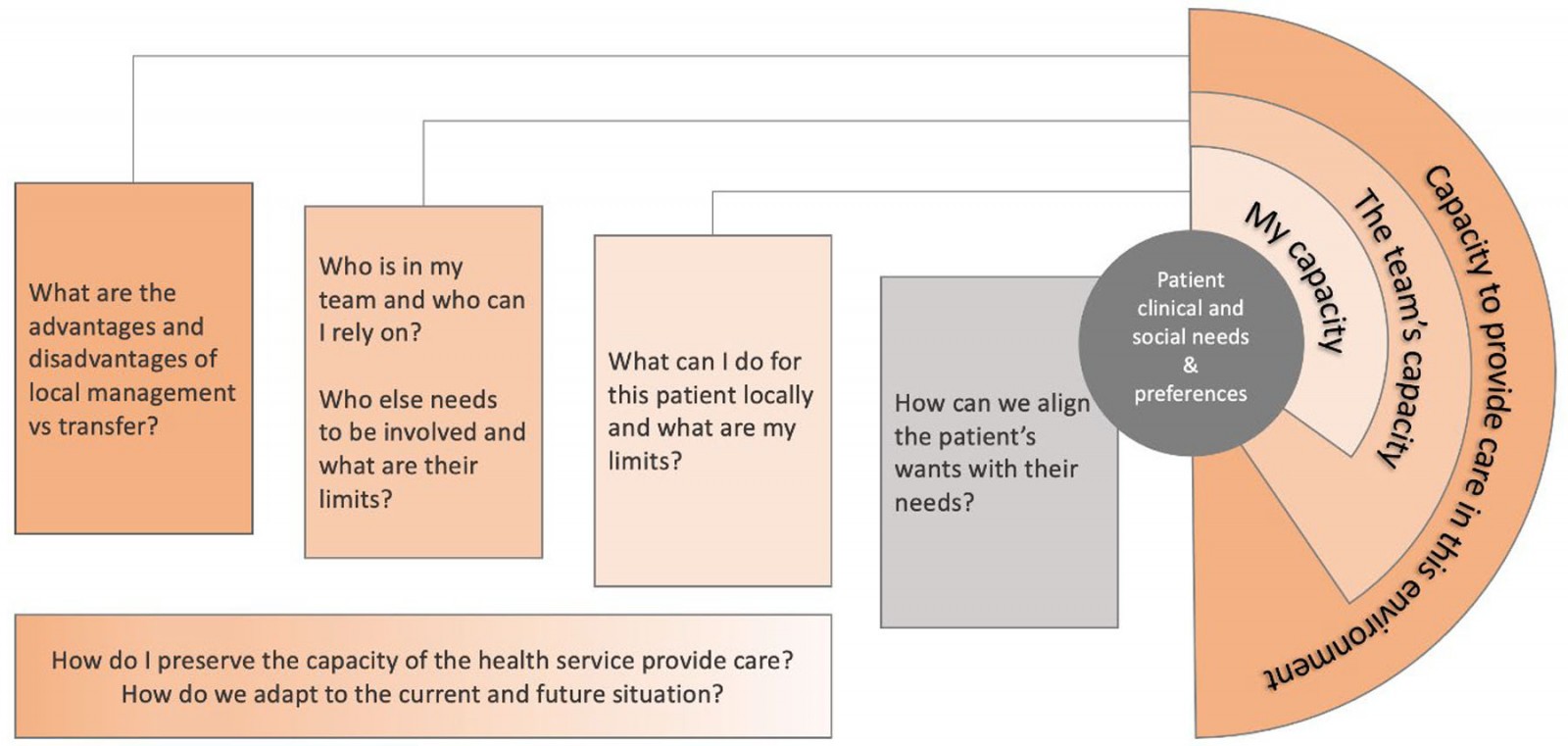 Figure 1: Pellegrini Therapeutic Reasoning Model – relationships between components.
Figure 1: Pellegrini Therapeutic Reasoning Model – relationships between components.
Limitations
There are several potential limitations with this study. All participants in the study were attendees at a workshop hosted by the Adelaide Rural Clinical School. As they are all associated with the same institution the data may reflect how this institution views therapeutic reasoning. Although the participants came from a variety of different settings, all work within South Australia, potentially reflecting how rural generalists work within the state. The presence of only a single scenario may have limited the breadth of data collected. We acknowledge that our model was developed within the limitations of a single simulation framework, and with a limited number of participants. Further studies will be required to evaluate the robustness of the model.
Conclusion
This study explored the therapeutic reasoning process of rural generalists in a simulated scenario in a small rural hospital emergency department. Novel aspects of the study included bespoke development of a unique simulation model to explore the therapeutic reasoning process in a rural context, and development of a mental model to describe how rural generalists made management decisions acknowledging complexity and uncertainty. This framework provides prompts to consider as a starting point when communicating with peers or providing education to trainees, and may also provide a starting point for debriefing about real-world or simulated clinical scenarios.
Acknowledgements
Funding for this research was provided by the Australian College of Rural and Remote Medicine.
Conflicts of interest
DP, LuW, LiW and JP all work as rural doctors, with DP, LiW and JP having emergency medicine responsibilities. LuW, LiW and JP all have leadership roles in rural medical undergraduate or vocational training. DP is a general practice academic registrar. Australian Rural Clinical Schools are funded through the Australian Government Rural Health Multidisciplinary Training grant scheme. Funding for this research was provided by the Australian College of Rural and Remote Medicine.
references:
Supplementary material is available on the live site https://www.rrh.org.au/journal/article/8365/#supplementary
You might also be interested in:
2018 - Transformation of medical education through Decentralised Training Platforms: a scoping review
2007 - Polyarticular septic arthritis following septic circumcision