Introduction
Since the 1990s, the Nepali-speaking Bhutanese community has been subject to the largest resettlement operation in the world1. Between 1865 and 1930, the Lhotshampas, a Nepali-speaking people, migrated from Nepal and India to the south of Bhutan, a process encouraged by the Bhutanese government1,2. Despite being allowed into Bhutan, there existed an ‘ethnic boundary’ between the Lhotshampa migrants and the Bhutanese, believed to have been implemented by the Bhutanese in order to protect Bhutanese culture1,3. Over time, ethnic tensions between the two communities grew, as language and cultural restrictions were placed upon the Lhotshampas. Eventually in the 1990s more than 100 000 Lhotshampas (herein referred to as Nepali-speaking Bhutanese) fled to refugee camps in Nepal following persecution and torture in southern Bhutan1. Here they experienced further violence, malnutrition and poor health living in refugee camps in Nepal for up to two decades4. In recent years, thousands of Nepali-speaking Bhutanese refugees have been resettled throughout the world, with more than 5000 resettled in rural and regional Australia5.
This historical context confirms that Nepali-speaking Bhutanese refugees have a pre-migration history of collective trauma through exposure to torture, separation from family members, forced displacement and loss of identity6. They have also endured post-migration resettlement stressors7,8. The accumulation of these stressors places Nepali-speaking Bhutanese refugees at significant risk of mental and physical ill-health, including post-traumatic stress disorder9. According to Herman’s trauma framework10, psychological trauma results from disconnection and disempowerment from others and can disrupt social systems of care, which maps onto the experiences of Nepali-speaking Bhutanese refugees. Herman suggests that the way in which recovery can occur is by rebuilding personal relationships and by restoring a sense of power and control among those traumatised10. However, after migration such recovery is challenging due to issues such as language barriers, family separation, financial stressors, unemployment and insufficient support from governments. These stressors effectively compound pre-migration trauma8 and further erode social networks and community supports11.
Given the pre- and post-migration trauma, it is unsurprising that chronic pain is common among this population. The lifetime prevalence of chronic pain among Nepali-speaking Bhutanese refugees is estimated to be 56%9 compared with 13% in the general Australian population12. Pain is defined as an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage13. Chronic pain is pain lasting or recurring longer than 3 months14 and is either a syndrome in its own right or a symptom of an underlying condition such as cancer13. The traditional biomedical approach to chronic pain has limitations15, which gave rise to the biopsychosocial model of understanding pain, emphasising the complex interplay of biological, psychological and social factors16,17. The sociopsychobio model proposed by Haslam et al reformulates the biopsychosocial model and asserts that foreground social factors such as class, inequality, structure and networks strongly influence psychology and, in turn, influence biology and health18. This sociopsychobio model may help explain the experience and modulation of chronic pain in the resettled Nepali-speaking Bhutanese population, as collective group experiences could influence psychological as well as biological health factors.
The association between trauma and chronic pain is well established9,19-21, and people who are traumatised are 2.7 times more likely to develop a somatic syndrome19,22,23. Van Ommeren et al documented a variety of traumatic experiences inflicted on Nepali-speaking Bhutanese refugees, including severe beatings, threats, humiliation, forced incongruent acts, social isolation, sleep deprivation and hygiene deprivation, postulating links between past traumatic events, mental illness and pain9. Among other cohorts of resettled refugees, pain is experienced as a symptom of exile, isolation from one’s community and is associated with memories of home24,25. Combined, these findings are consistent with Haslam et al’s sociopsychobio model18, suggesting that various forms of cultural and social disruption may be associated with psychological distress and chronic pain among refugee cohorts.
Cultural disruption appears to be particularly important in determining refugee health outcomes. Culture encompasses intergenerational traditions and beliefs, as well as values and attitudes toward many aspects of life including spirituality, family, death and health care26. Culture can influence the communication and expression of pain, tolerance of pain, as well as beliefs about coping with pain27-30. Given that pain can be viewed and expressed differently by different cultures, Western pain management programs may not be meeting the needs of migrant groups31,32. Brady et al found that, across three distinct cultural groups in Australia (Mandaen, Assyrian and Vietnamese), pain was conceptualised through biomedical, biopsychosocial or traditional medicine approaches, and pain conceptualisations were influenced by gender, ethnicity, religion, and community or group membership31.
Past research has examined cultural aspects of general coping among Nepali-speaking Bhutanese refugees while in refugee camps33, but how they coped with pain was not documented. The authors suggest that participants favoured active problem-solving approaches to coping (positive reframing, planning), as well as culturally approved help-seeking behaviours (meditation, religious practices, acceptance and distraction). Among resettled Nepali-speaking Bhutanese refugees in the US, informal social support networks, including relatives, neighbours, friends and other community members, were considered central to managing distress and suicidality34. Some research also indicates that peer-led interventions may be helpful for the resettled Nepali-speaking Bhutanese people in the US in order to provide a sense of community, belonging and unity35.
Despite the profound effects of trauma and displacement on the health of resettled Nepali-speaking Bhutanese people, few studies have investigated their experiences of chronic pain. There is emerging research on the conceptualisations of mental health among this population8, but to our knowledge there have been no studies exploring how resettled Nepali-speaking Bhutanese people conceptualise pain. We aimed to conduct a qualitative study to explore conceptualisations and beliefs about pain held by the Nepali-speaking Bhutanese community in rural and regional Australia.
Methods
Study design
Qualitative focus groups were used, allowing a collaborative exploration of pain within a social framework that would not have been possible through individual interviews36. Focus groups yield rich data and groups can empower individuals who may otherwise be marginalised; they also allow the collection of data from those who are not literate36,37.
The focus groups were facilitated by a Nepali-speaking Bhutanese female, who relocated to Australia in 2009 following 18 years at a refugee camp in Nepal. The facilitator has been a trusted figure among a Nepali-speaking Bhutanese community in regional Australia since 2014. She works as a qualified interpreter at a primary care clinic, providing interpreting services for the Nepali-speaking Bhutanese community, as well as facilitating groups on women’s health and cultural adaptation. Prior to her work in Australia, she had worked as a teacher and nursing assistant in refugee camps in Nepal. The use of a community member is beneficial in research to promote better engagement and trust with participants, allowing rich and meaningful data to emerge36,38.
Participants
Participants were recruited through a primary care clinic in regional Victoria, which has ties to a statewide pain clinic in Melbourne. A total of 32 patients were invited to participate. Four declined and five moved interstate, making them ineligible. Eligible patients were mailed a Nepali language version of the Participant Information and Consent Form (PICF) as well as an audio-recording of the PICF in Nepali. Those interested were invited to attend one of three focus groups. Eligibility criteria were: age ≥18 years, previous settlement in refugee camps in Nepal, subsequent resettlement in Australia and self-report of chronic pain.
Procedure
Three focus groups (seven males, seven females and eight females, respectively) were conducted in April 2019, each lasting approximately 1.5 hours. Focus groups were allocated based on gender, which the bilingual facilitator suggested was most culturally appropriate. The bilingual facilitator was provided 2 hours of training on how to facilitate focus groups. In addition to this, as part of her role as interpreter, she had previously undergone training in group facilitation and translation. Individual taxi vouchers were used to transport participants to and from the clinic and $20 vouchers were provided as a gesture of thanks to participants.
Upon arrival, participants individually met with the bilingual facilitator and a researcher to re-read the PICF and to ask questions about the study before providing signed consent. The demographics questionnaire was then completed, which included questions about age, gender, education and pain. Additional demographic information regarding religion, medical and psychiatric diagnoses was accessed from the medical database at the pain clinic. The focus groups were conducted in Nepali by the bilingual facilitator, using the semi-structured focus group schedule, and all sessions were audio-recorded. Three researchers were also present in the room to take notes and assist the facilitator where appropriate.
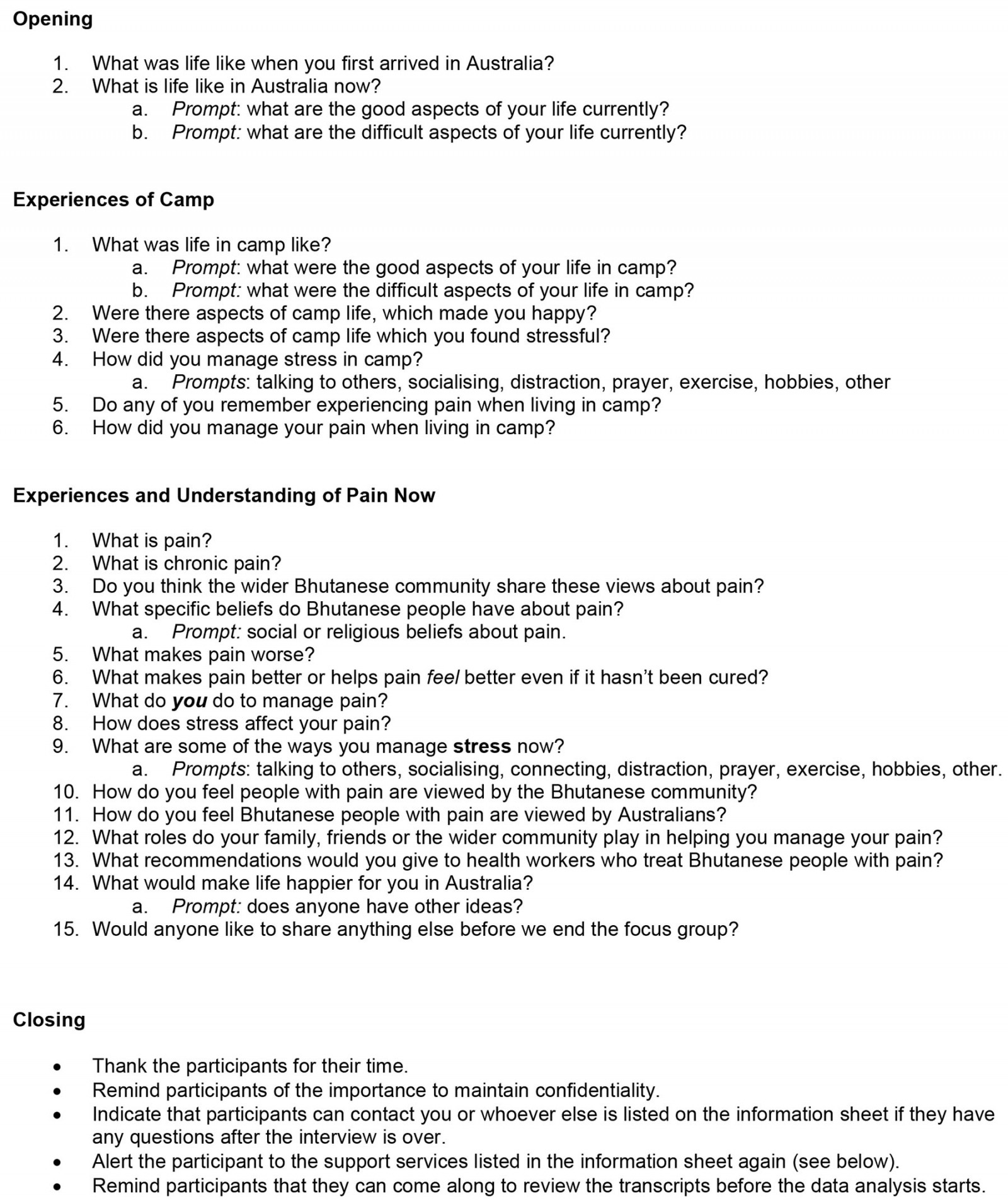
The interview schedule was created by the researchers to guide the topics of the focus groups (Appendix I). In the design phase of the study, focus group questions were discussed with the bilingual facilitator to ensure they were culturally appropriate, and changes were made where necessary. The interview schedule began with general introductions to build rapport, and then detailed the nature of the study and an overview of the focus group. The interview included questions regarding the participants’ experiences in the refugee camp, their life in Australia, and their experiences and beliefs regarding their pain.
Data processing and analysis
The audio-recordings were transcribed and translated by an Australian translation service, Translationz. The data were first transcribed in Nepali and were subsequently translated to English; the interpreter and translator involved was accredited by the National Accreditation Authority for Translators and Interpreters. The bilingual facilitator then verified these translations. Once translated, researchers began the process of a thematic analysis39. Two researchers performed the thematic analysis; their analyses were informed by the sociopsychobio theoretical framework18, as well as their academic and clinical psychology training. The analysis was completed using a predominantly inductive approach; however, by using a semi-structured focus group schedule, there was also a deductive approach to the analysis as the questions were designed to explore a particular focus. The analysis was completed across the entire dataset to identify commonalities within the dataset as a whole. Initially, two researchers independently coded the transcripts, focusing on finding meaning and patterns within the data to generate initial codes.
A coding frame was developed from the first two transcripts by consolidating all of the researchers’ independent codes. A number of utterances were found to be difficult to code due to issues where the direct translation was unclear due to differences in linguistic context between Nepali and English. However, these discrepancies were rectified by consulting the bilingual facilitator who provided further context and explanation of the translations so the correct meaning could be ascertained.
The coding frame was also reviewed by a third researcher to ensure its utility before being used to code the final transcript. Both researchers independently coded the third transcript, and a reliability analysis was conducted to determine the level of consistency between the two researchers. The reliability analysis revealed that, of the 136 codes in the third transcript, 128 were agreed upon by the two researchers. This included 79 consistent codes between the researchers and an additional 49 codes that were agreed upon through discussion. Two disagreements between the researchers were resolved by discussion with the bilingual facilitator and six codes were also deleted from the transcripts. Cohen’s k was used to calculate reliability, which resulted in k=0.85, suggesting strong reliability. The coding frame was then adjusted to account for developments following the reliability check, and transcripts 1 and 2 were reviewed again to account for revisions to the coding frame.
Two researchers independently conducted a thematic analysis by assessing the similarity of codes and generating clusters of codes to determine themes. Once complete, each of the researcher’s themes were discussed and consolidated, until five final themes were agreed upon, as shown in Figure 1.
After themes were determined, a feedback session via videoconferencing was held with the participants to present the overall themes and ensure that they represented what the participants had intended to say. Sixteen of 22 participants attended the feedback session and participants noted agreement across all five themes.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Human Research Ethics Committee (HREC) at St Vincent’s Hospital Melbourne (HREC 189.18; 20 March 2019).
Results
Participant characteristics
Twenty-two eligible patients agreed to participate (15 females and 7 males). At the time of the study, all participants were residing in rural and regional Australia. Participants were aged between 30 and 65 years (mean (M)=49.81, standard deviation (SD)=8.84), had been living in Australia between 2 and 11 years (M=6.36, SD=2.83) and had been experiencing chronic pain for between 2 and 33 years (M=10.22 years, SD=7.09). Sixty-five per cent of participants were experiencing widespread pain and 35% had pain in specific sites, most commonly in the lower back, shoulders, head and knees. Forty-three per cent had at least one mental health disorder such as post-traumatic stress disorder, depression, anxiety or psychosis. In addition to chronic pain, all participants also experienced at least one comorbid chronic illness. All participants were unemployed, either due to pain or another medical condition. Twenty (86%) participants had no formal education while the remaining three (13%) participants had primary school education only. The majority of participants (86%) were practising Hindus, while the religion of the remaining three (13%) participants was unknown. Some participants had Australian citizenship, the percentage of which was not collected.
Five themes were developed from the focus group data: (1) pain is persistent and creates suffering, (2) pain is subjective and poorly understood, (3) pain is a biomedical problem that needs to be solved, (4) pain is complex and more than a biomedical problem, and (5) coping with pain is multi-faceted (Fig1). Selected quotations are presented in Table 1.
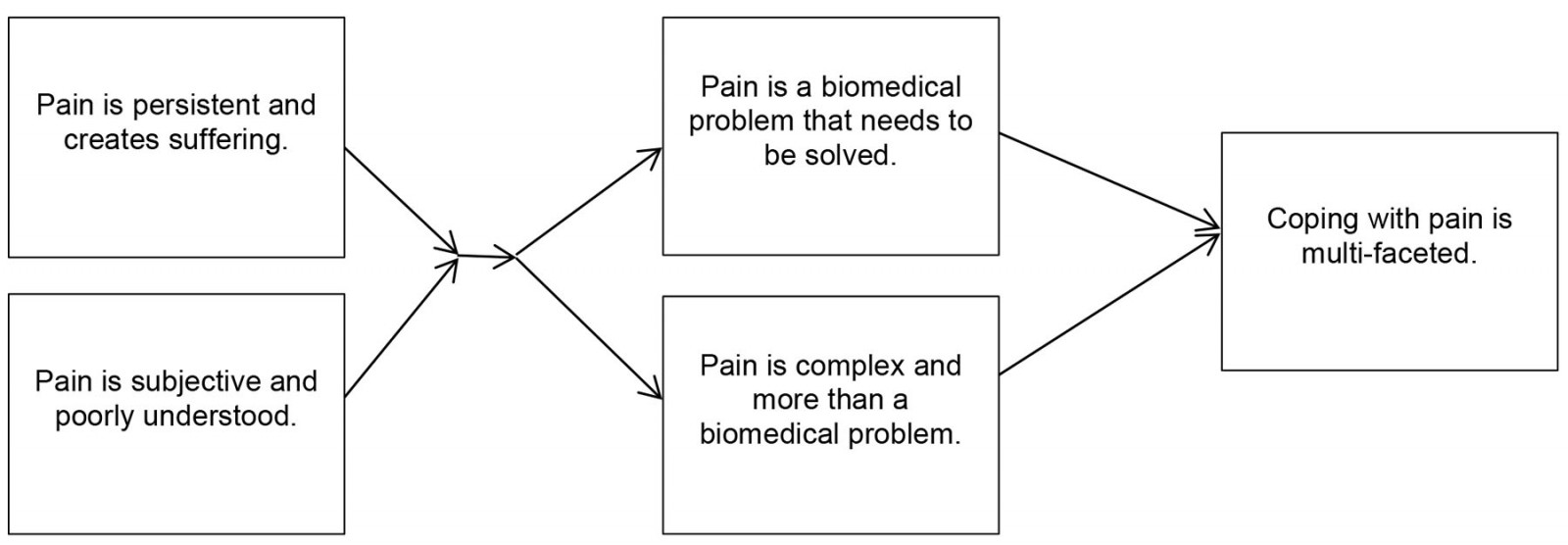 Figure 1: Thematic map of participant responses.
Figure 1: Thematic map of participant responses.
Theme 1: Pain is persistent and creates suffering
Participants identified that pain was persistent and created suffering. Three participants reported that, due to the persistent nature of their symptoms, they believed their pain was incurable. Many participants reported that their pain had not improved since accessing treatment in Australia and, for some, pain had worsened and spread to other areas of their body. Three participants reported that their suffering had increased since arriving in Australia. The participants’ persistent pain resulted in functional impairments such as limiting walking, sitting, standing, cooking, working, studying and driving. These impairments created further suffering and made it more difficult to manage everyday life. One participant noted that the pain reduced their confidence and autonomy, greatly disrupting their ability to manage everyday tasks.
Theme 2: Pain is subjective and poorly understood
The second overarching theme was that pain was a personal and subjective experience that was poorly understood by others. Some participants believed that persistent pain could only be understood by those who had experienced it. In general, participants said that their persistent symptoms were poorly understood by the medical community, government agencies, their peers and the wider Australian community, leading to stigmatisation and judgement from others. Four participants identified feeling invalidated by the medical community – sometimes being scolded by doctors, not being allowed time to speak, experiencing ethnic discrimination and feeling that doctors were frustrated with them. However, invalidation was not common to all, as two participants noted that they had been treated positively by doctors and had trust in the medical community. Some participants described feeling judged for not being able to work and expressed that their peers, from both Nepali-speaking Bhutanese and Australian communities, did not believe their pain and felt they were feigning pain for financial incentives. Participants also felt that the nature of their conditions was not understood by government agencies, citing unreasonable expectations from employment agencies and social welfare to find work, and that these pressures increased their suffering and pain.
English language barriers were key issues participants faced when describing their pain to others. The participants felt that they could not communicate their pain in English effectively. They were also concerned that their words may not be translated properly to their doctors. Additionally, it was noted by the bilingual facilitator that, when speaking Nepali, participants tended to use some words broadly, such as the term ‘doctor’ when referring to any health professional, and other terms were used interchangeably such as ‘suffering’ and ‘pain’. They also expressed that doctors did not fully understand the nature of their persisting symptoms and perceived that doctors were prescribing medications on a trial-and-error basis. Poor communication worked both ways: participants identified they did not understand the underlying causes of their pain or why treatments were not working, due to ineffective communication by their doctors. One participant expressed the hope for pain to be measured objectively with a machine to aid assessment and treatment and remove the doctor’s ‘guessing’.
Theme 3: Pain is a biomedical problem that needs to be solved
Many participants described the source of their persistent pain using biomedical language. For example, some participants said that their pain was the result of a disease or serious injury. Other participants theorised that their pain was linked to malnutrition or a failure to be vaccinated in refugee camps, leading to diseases that were now causing pain. Within this biomedical view of pain, five participants expressed the belief that medication was the only treatment for their pain. However, five participants questioned whether long-term medication use could lead to further medical problems. Participants often took a mechanistic view of their pain: pain was a problem that was caused by a disease that, if doctors diagnosed quickly, could be treated, thus reducing or curing their pain and suffering.
Theme 4: Pain is complex and more than a biomedical problem
Many participants expressed views that were inconsistent with biomedical conceptualisations of pain, instead identifying affective, social, cognitive and environmental factors influencing pain. This included discussion of the relationships between depression, anxiety and stress with pain, and the subsequent effects emotions have on the body such as tension and bowel or bladder dysfunction. External stressors relating to finances were also mentioned as contributors to pain. Participants discussed how traumatic memories could trigger feelings of pain, lead to a sense of disconnection from the body and impact the soul. Participants spent time recounting traumatic experiences in the refugee camps, including fires, the destruction of their belongings, having no income, and the lack of food, electricity and water. Participants said that recollections of such events still brought them pain. The influence of social interactions on pain was also discussed. Participants noted that stigma and judgement from others could also result in pain. One participant said that they believed the doctor’s role was not simply to prescribe medication, but also to hear the patient’s experiences and concerns.
Theme 5: Coping with pain is multi-faceted
Participants reported using a variety of physical, social and psychological coping strategies to manage their pain in the short term. These included passive aids such as heat and massage, as well as active aids such as hydrotherapy, exercise, relaxation and meditation. However, participants reported that financial pressures precluded them from engaging with these pain management strategies. Participants also described how social and cultural engagement, such as talking to friends, speaking their own language or attending religious festivals, distracted them from their pain, providing short-term relief. However, a few participants reported that social engagements could increase their pain due to perceived judgement and associated stigma, making social engagement an unreliable pain relief strategy. Some participants said that employment would lessen their pain; however, they found applying for jobs difficult due to literacy issues, language barriers and fear of judgement.
Overall, many participants engaged in both active and passive strategies for pain management, some of which were culturally informed, but access to relevant resources was impacted by social deprivation. Two participants reported that their pain had improved since arriving in Australia, but most found these pain management strategies limited, as they neither provided long-term relief, nor a cure.
Table 1: Study themes and selected participant quotations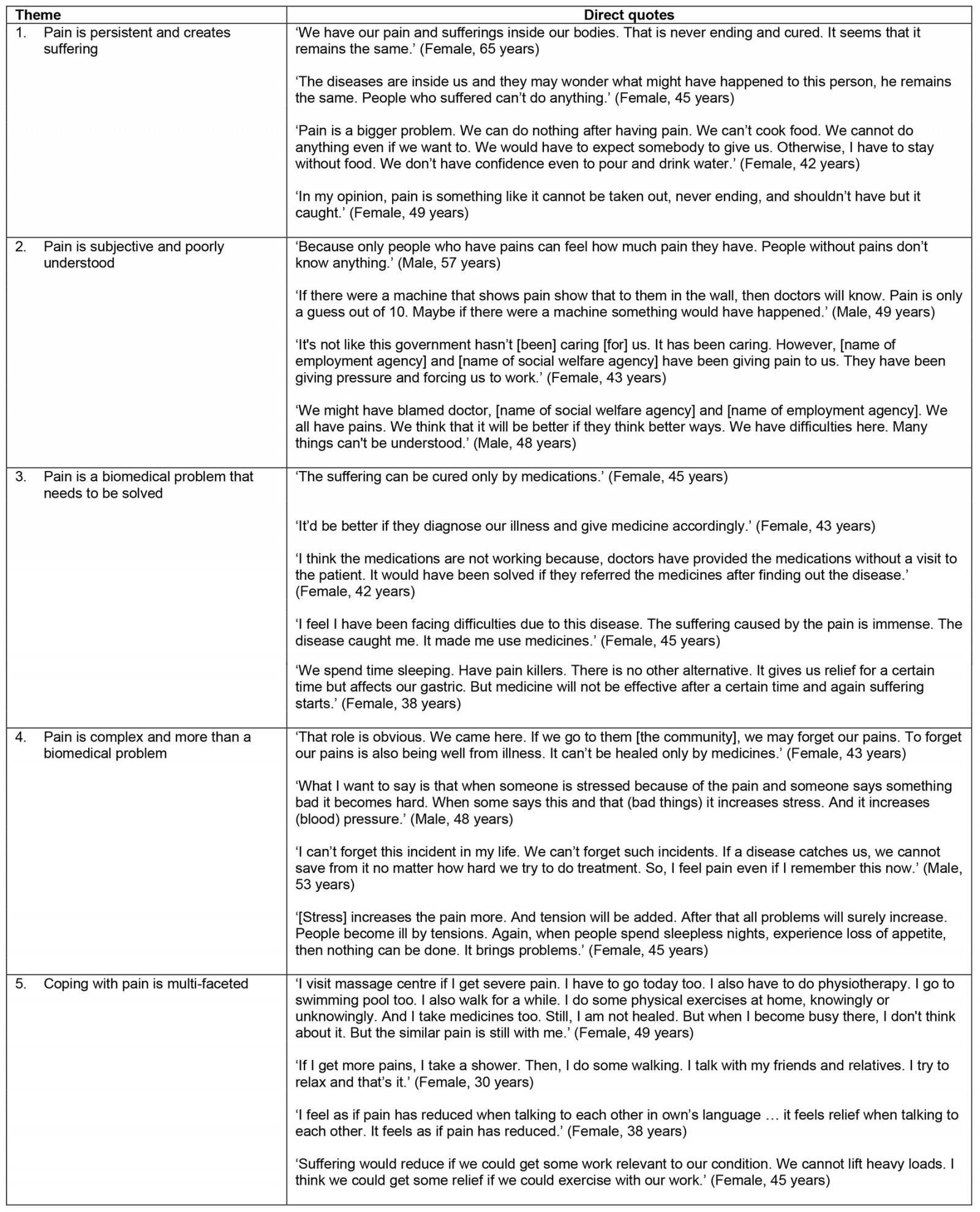
Discussion
Qualitative focus groups were used to explore conceptualisations and beliefs about pain held by members of the Nepali-speaking Bhutanese community in rural and regional Australia. There is a paucity of research in the area and rates of chronic pain among this population are high. The key findings suggest that pain is persistent and creates suffering, pain is subjective and poorly understood, pain is a biomedical problem that needs to be solved, pain is complex and more than a biomedical problem and coping with pain is multi-faceted. This study adds to the growing refugee health literature and gives voice to some of the issues and beliefs held by a subsection of individuals from the Nepali-speaking Bhutanese community in rural and regional Australia.
A common experience for all participants was that pain was persistent, viewed in a negative light, increased suffering and made life in Australia harder. Chronic pain persists or recurs for longer than 3 months14 and participants understood its long-term nature. Some participants noted how pain had worsened over time and how the pain had spread to different body parts, as happens in chronic pain syndromes40. Some participants used the words ‘pain’ and ‘suffering’ interchangeably, suggesting that suffering was inherent in the experience of pain. Three participants said their suffering had increased since moving to Australia. The exact reasons for this were not explored in the focus groups; however, it is hypothesised that social factors, such as interactions with government agencies, communication challenges with healthcare workers, stigma and financial stress among others, may have had adverse impacts on some participants’ pain experiences. Moreover, the participants commented on how pain impacts their everyday function and their psychological wellbeing, and these impacts are also emphasised in the revised definition of pain13. Interestingly, no participants referenced the adaptive role of pain, and focused only aversive impacts. Western pain education programs, particularly in Australia, teach the concept that chronic pain is a protector and not an accurate indicator of tissue damage41, intended to reduce catastrophising and enhance understanding of pain from a biopsychosocial perspective. It is unclear how such pain education would be understood by the participants, and this requires further research.
Participants viewed pain as subjective and something that could only be understood by someone who had experienced similar pain. This made participants feel disconnected from healthcare workers, who they assumed may not have had the same lived experiences of chronic pain, social isolation and pain invalidation. It also put pressure on participants to explain and justify their pain to healthcare workers, which was difficult because of language barriers. Participants repeatedly said they did not feel heard or understood by healthcare workers, Australian and Nepali-speaking Bhutanese communities alike, perpetuating feelings of stigmatisation and judgement. Previous research has shown that Nepali-speaking Bhutanese people rely on informal social support networks as a coping strategy34, thus barriers to expressing pain and feeling misunderstood by others place the participants at risk of significant social isolation and likely impede the management of both pain and trauma.
Findings also suggested that positive interactions with healthcare workers could improve participants’ experiences. Participants expressed frustration with health professionals for not adequately listening or not giving a correct diagnosis, which many believed led to poor treatment efficacy. From the patients’ medical records, many had a primary pain diagnosis, meaning that their pain was not a symptom of another disease. It is likely that there is a bidirectional miscommunication occurring between the participants and doctors, as participants did not seem to understand that chronic primary pain is a diagnosis in itself42. These findings were in line with previous research findings that many refugees faced communication and cultural barriers within healthcare settings7,8,43. Participants suggested that healthcare workers should take more time to listen to their stories, as this may be therapeutic in itself29, and it aligns with cultural humility, wherein one sensitively listens to patients and appreciates their individualised cultural experiences44,45. This openness to hearing individual stories may then be helpful to provide further education about chronic primary pain in a culturally informed way, akin to the ecological validity model by Bernal et al46, that could draw upon metaphors and imagery familiar to the individual. According to participants, other ways to improve health care included access to interpreters to facilitate a thorough assessment, explain diagnoses clearly and instil hope. These recommendations provide valuable insights when designing future assessment guidelines and treatment programs for this population, which may improve healthcare inequalities.
Some participants conceptualised pain in a biomedical way, believing chronic pain to be a result of a disease or injury. Part of this was a mechanistic way to solving their pain: a ‘correct’ diagnosis is followed by specific effective treatment and medication that would relieve or cure the pain. This mechanistic approach to problem-solving has previously been reported as a general coping strategy among Nepali-speaking Bhutanese refugees33. Consequently, biomedical and mechanistic conceptualisations of pain are to be expected among Nepali-speaking Bhutanese people, and whether these beliefs are modifiable through pain education remains unknown.
While the biomedical view of pain was common, other participants recognised that psychosocial factors also influenced pain. This included the impact of social judgement, isolation, traumatic memories and financial burden, which supports previous research24. These findings indicate that some participants hold views of pain that are beyond biomedical conceptualisation15 and more in line with a sociopsychobio perspective18. One of the most frequent discussions across the focus groups was that participants found biomedical management to be limited or ineffective, especially when the pain diagnosis excluded a sense of feeling heard. Thus, some individuals may be more open to active self-management for pain, which should be founded on an appreciation of the impact of cultural context, social injustice and historical trauma on pain. Emphasis should also be placed on the management of chronic pain rather than seeking a cure due to the long-term nature of primary pain42.
It should be noted that biomedical conceptualisations of pain are not unique to the Nepali-speaking Bhutanese; these beliefs are also found in cohorts of Western societies47-49. Anecdotally, we observe varying pain beliefs at the tertiary pain clinic where this research was conducted, whereby service users hold biomedical, psychosocial or biopsychosocial beliefs about pain. Thus, there is some alignment between the varying views held by the Nepali-speaking Bhutanese and what we typically observe in the clinic. With the dissemination of evidence-based pain education and self-management skills through public health campaigns such as that of Buchbinder et al50, public attitudes towards a non-biomedical model of pain are developing in Australia. It is unclear whether the psychosocial perspectives of pain held by the participants are related to acculturation to Australia or whether these beliefs pre-dated resettlement.
We found that participants engaged in both active and passive strategies for pain management, some of which were culturally informed, such as spending time with the community, speaking in their native language and attending religious festivals. This supports previous research conducted with other migrant groups in Australia31, and suggests that culturally aligned coping mechanisms are important for the Nepali-speaking Bhutanese community. Participants also endorsed other forms of active coping such as physiotherapy and hydrotherapy, indicating a willingness to engage in movement-based pain management. However, access to pain management resources was limited due to financial barriers.
The present study used multiple reliability checks, which strengthens the validity of the data. It also had a high uptake of participants, which allowed many members of the community to voice their experiences. A non-random purposive sample was used for this study given the challenges of reaching and working with this population. While this has provided an excellent depth of data, the findings are not intended to and do not represent the entire Nepali-speaking Bhutanese community and thus cannot be generalised to broader groups. Additionally, while the use of focus groups allowed a collaborative exploration of pain, limitations of focus groups such as social desirability and concerns over confidentiality may have influenced participant responses36,51.
Difficulties also emerged in analysis, due to the quality of translation. The transcripts contained some grammatical errors, leading to issues with interpretation. As the quotes are translations only, some meaning and richness may have been lost in this process, but this limitation is not unique to the present study8. Grammatical issues were rectified by consulting the bilingual facilitator, and the feedback session with participants was also held to verify the accuracy of the translations; however, a formal independent back-translation from English to Nepali would have been useful.
It was expected that responses from the focus groups would emphasise more cultural and religious views, similar to other studies31. This may be due to limitations of the interview schedule, which did not directly ask about specific cultural, religious or spiritual beliefs, due to its predominantly inductive approach; previous research has indicated that people from refugee backgrounds prefer to be asked direct questions in healthcare settings43. This is important for future research as there may be underlying cultural nuances in the conceptualisations of chronic pain that were not represented in this study.
Conclusion
A cohort of Nepali-speaking Bhutanese people living in rural and regional Australia conceptualised chronic pain as persistent, subjective and poorly understood. Some participants viewed pain through a predominantly biomedical lens, and some recognised social and psychological factors as contributors to pain, such as social injustice and traumatic memories. Overwhelmingly, the participants believed pain is complex and multifaceted, requiring active and passive strategies for management, some of which are culturally informed. The findings may assist local healthcare practitioners to understand some of the common beliefs about pain, and the barriers to communicating pain among resettled Nepali-speaking Bhutanese people in rural and regional Australia. Appreciation for cultural humility, historical trauma and careful attention to an individual’s pain story is warranted when assessing and supporting Nepali-speaking Bhutanese people with chronic pain. Multi-site international research would help to understand the similarities and differences in how pain is conceptualised by Nepali-speaking Bhutanese people resettled in other countries. Future research should focus on the development of culturally and trauma-informed pain education, and to evaluate whether such interventions can modulate the pain experience.
Funding
The study was funded by a Research Endowment Fund grant from St Vincent’s Hospital Melbourne (REF 88231) awarded on 14 December 2018.
Conflicts of interest
The authors have no conflicts of interest to disclose.
References
You might also be interested in:
2022 - Experiences of rural and remote nurses during and following disasters: a scoping review