Introduction
Salmonella spp. is one of the most commonly reported causal agents of bacterial gastroenteritis and a leading cause of foodborne outbreaks globally1. Several modes of transmission of this bacteria have been implicated; however, an estimated 94% of salmonellosis is transmitted via contaminated food mainly of animal origin2 such as poultry and pig meat, eggs and milk3-5. According to the White–Kauffmann–Le Minor scheme6, more than 2500 serotypes have been identified. Salmonella enterica subsp. enterica serovar Give (S. Give), with antigenic formula (3,10:l,v:1,7), is one of the less frequently isolated serotypes in humans: between 2007 and 2021, 1874 S. Give cases, in total, were reported in EU and European Economic Area (EEA) countries7,8. Foodborne outbreaks due to this serotype occurred in Germany in 2004, linked to the consumption of raw pork minced meat9; in France in 2008, linked to infant milk formula; and in Malta in 201610,11. In Greece, for the same period, only eight sporadic cases were identified12.
Human salmonellosis is one of the mandatory notifiable diseases in Greece through the Mandatory Notification System administered by the National Public Health Organization (NPHO). Human Salmonella isolates are sent to the National Reference Laboratory for Salmonella (Salmonella NRL) on a voluntary basis12.
Historical data: S. Give outbreak, region A, southern Greece, 2018
In July 2018, 15 gastroenteritis cases were reported at the NPHO in residents of region A, a rural area of southern of Greece, far away from the main town of the area. Salmonella spp. isolates isolated from stools of six patients were sent to the Salmonella NRL and were serotyped as Salmonella enterica enterica serotype Give. According to the descriptive epidemiological investigation, for 12 cases with available information, the date of symptom onset was 2 July 2018. The median age of cases was 31.5 years (range 7–65 years); 46.7% of cases were female. All cases (n=15) demonstrated diarrhea as the main symptom. Nine patients developed fever (>38ºC) and vomiting. Six (40%) patients were hospitalized. The median age of hospitalized patients was 16 years (range: 7–53 years). All patients had consumed a local traditional recipe of roasted pork meat purchased from a restaurant in region A.
One of the S. Give patients was the owner of the restaurant, who was also involved in the procedure of cutting the roasted pork meat into slices. Leftovers from the pork meat tested positive for S. Give. Traceback and veterinary investigations did not identify any S. Give positive samples on surfaces, or in swine carcasses at the slaughterhouse of the livestock unit from where pork meat was supplied. However, environmental investigation revealed that the restaurant purchased the pork already roasted from another shop in the same region. Νon-compliances with food safety measures (eg violation of food preservation temperature) were identified in the pork distribution process, and correctional measures were implemented.
A few days earlier, in June 2018, the same restaurant was implicated, with a cluster of 10 gastroenteritis cases reported to the NPHO. Epidemiological investigation again revealed consumption of roasted pork meat. A stool sample collected from one patient was positive for Salmonella spp.; Salmonella isolate was not sent to the Salmonella NRL for serotyping. By the time of notification, leftover food samples were not available for further laboratory investigation.
In addition, one sporadic S. Give case and a cluster of three gastroenteritis cases (one of the isolates was sent to the Salmonella NRL and serotyped as S. Give), were reported in June and September 2018, respectively. The food consumption history of roasted pork meat purchased from food street vendors in local festivals in region A was identified.
Alert for a new S. Give outbreak, region A, southern Greece, 2022
In September 2022 a cluster of 10 gastroenteritis cases was reported to the NPHO by a healthcare center in region A regarding residents of region A. According to preliminary information, all the cases had diarrhea, with a reported date of symptom onset of 12 September 2022. According to their food consumption history, they all had consumed roasted pork meat on the 11 September, purchased from a food street vendor during a local religious festival in region A.
Study aim
The aim of the study is to present the results of the investigation of the outbreak reported in September 2022 in region A of southern Greece in relation to cases of 2018, which presented similar characteristics (same rural region A, same implicated food vehicle), attributed to S. Give.
Methods
Epidemiological investigation – active case finding
To investigate the outbreak, a descriptive epidemiological investigation was conducted. The NPHO contacted directors of the local healthcare facilities and in other regions that also reported cases linked with the event. The aforementioned healthcare facilities were asked to report all gastroenteritis cases and their descriptive data: age, gender, place of exposure, information on symptoms, day and time of symptom onset and hospitalization status. In parallel, during preliminary laboratory investigations, Salmonella spp. was isolated in stool samples of cases and serotyped as S. Give. Therefore, all the implicated healthcare facilities were requested to notify any new salmonellosis cases, linked to the local religious festival in region A on 11 September 2022, via the Mandatory Notification System and send Salmonella isolates to the Salmonella NRL.
Involved healthcare facilities with no Salmonella testing laboratory capacity were requested to send stool samples to the Central Public Health Laboratory, where screening for 22 different enteropathogens was applied by multiplex PCR. Due to the extent of this social event, in which a large number of people from neighboring areas of region A participated, we informed all the healthcare facilities of the possibly affected areas, to report any gastroenteritis cases with pork meat consumption history in the specific event or anywhere else.
Confirmed non-typhoidal salmonellosis cases were defined as any person who attended the local religious festival on 11 September 2022, and during 11–17 September 2022 had three or more daily diarrheal episodes, and a stool sample positive for S. Give.
Probable non-typhoidal salmonellosis cases were defined as any person who attended the local religious festival on 11 September 2022, and during 11–17 September 2022 had three or more daily diarrheal episodes, and a stool sample positive for Salmonella spp.
Possible non-typhoidal salmonellosis cases were defined as any person who attended the local religious festival on 11 September 2022, and during 11–17 September 2022 had three or more daily diarrheal episodes.
A semi-structured questionnaire was designed and used for data collection through phone interviews with patients.
Leftovers of roasted pork meat were sent to the Central Public Health Laboratory for Salmonella detection.
Laboratory investigations
Serotyping for the identification of somatic antigen O and flagellar antigen H (phases 1 and 2) was performed by the slide agglutination method, according to the White–Kaufmann–Le Minor Scheme6. Susceptibility testing was performed on all S. Give isolates – human and food source – by the agar disk diffusion method (Kirby–Bauer) according to the protocols and guidelines of the European Committee on Antimicrobial Susceptibility Testing—EUCAST13 . The following antibiotics (Oxoid™ Antimicrobial Susceptibility discs, Thermo Scientific, https://www.thermofisher.com) were tested: ampicillin (A), amoxicillin–clavulanic acid, ceftazidime, cefotaxime, ciprofloxacin, chloramphenicol (C), tobramycin, netilmicin, nalidixic acid (Na), pefloxacin, streptomycin (S), sulphamethoxazole (Su), tetracycline (T), trimethoprim (Tm) and sulfamethoxazole–trimethoprim. Antimicrobial susceptibility testing was performed for human and food S. Give isolates. Molecular typing was performed by applying pulsed field gel electrophoresis of genomic DNA with XbaI according to the PulseNet protocol14. Fingerprints were analyzed using Bionumerics v6.6 (Applied Maths; https://www.applied-maths.com). Dendrograms were constructed using the Dice similarity coefficient and the unweighted pair group method with arithmetic averages, with optimization and position tolerance set at 0.5% and 1.5%, respectively. Pulsed-field gel electrophorese (PFGE) was performed for human and food isolates of both S. Give outbreaks (of 2018 and 2022) (Table 1). Sporadic S. Give human isolates (n=2 isolated in 2016 and n=1 isolated in 2017) delivered to the Salmonella NRL from healthcare facilities of region A were also included. Two epidemiologically non-related S. Give isolates were also tested in order to ensure the discriminatory power of PFGE on the specific serotype.
Table 1: Data on sporadic and outbreak gastroenteritis/Salmonella spp/Salmonella Give cases linked to consumption of roasted pork meat, region A, southern Greece, 2018 and 2022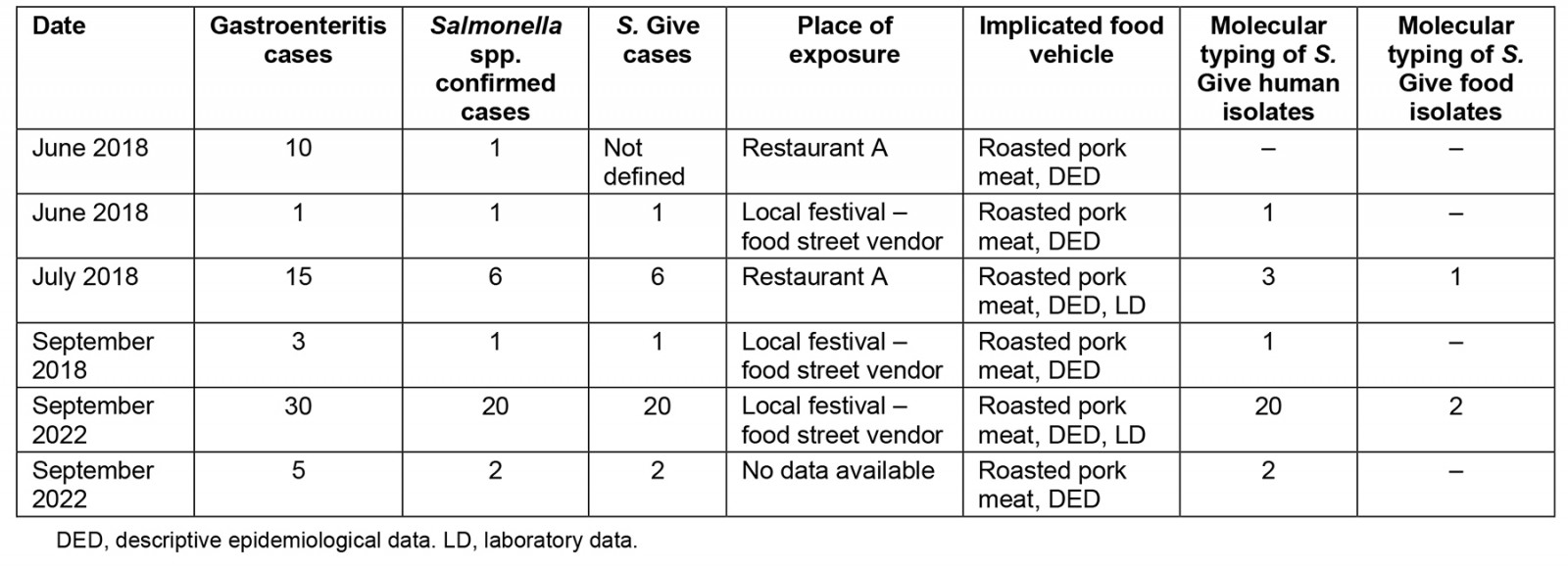
Environmental investigation
The NPHO informed the local public health authority, the food safety authority and the local veterinary authority about the ongoing outbreak. During the preliminary interviews with the cases, it was apparent that they had purchased the implicated roasted pork meat from a food street vendor at the local religious festival. Thus, the three authorities were requested to inspect the premises where the food item was prepared and cooked, collect stool samples from the food handlers involved in food preparation, collect equipment and surface samples from the premises and the vehicle that was used for the handling of the pork meat, search for food samples, and conduct a traceback investigation.
Ethics approval
Ethics approval was received by the Hellenic National Public Health Organization (Review Board Statement: Approval number: NPHO-25409/28-12-2022).
Results
Epidemiological investigation
Between 11 and 17 September 2022, 30 cases of acute gastroenteritis were reported by participants of the local festival. Twenty out of the 30 were non-typhoidal salmonellosis cases. For two cases the date of symptom onset was not available (Fig1). The median age of the 30 cases was 40.5 years (range 3–85 years); 53.5% of cases were male. Symptoms of patients included diarrhea (100%), fever (>38ºC; 70%) and vomiting (53%). Seventeen (57%) patients were hospitalized. The median age of hospitalized cases was 34 years (range 3–55 years). All cases had consumed roasted pork meat that had been purchased from the local festival. Since region A is far away from the main town of the area (about 52 km), cases were dispersed in six different healthcare facilities in seeking medical care: two healthcare facilities around the main town of the area and four in Athens, the capital city of Greece.
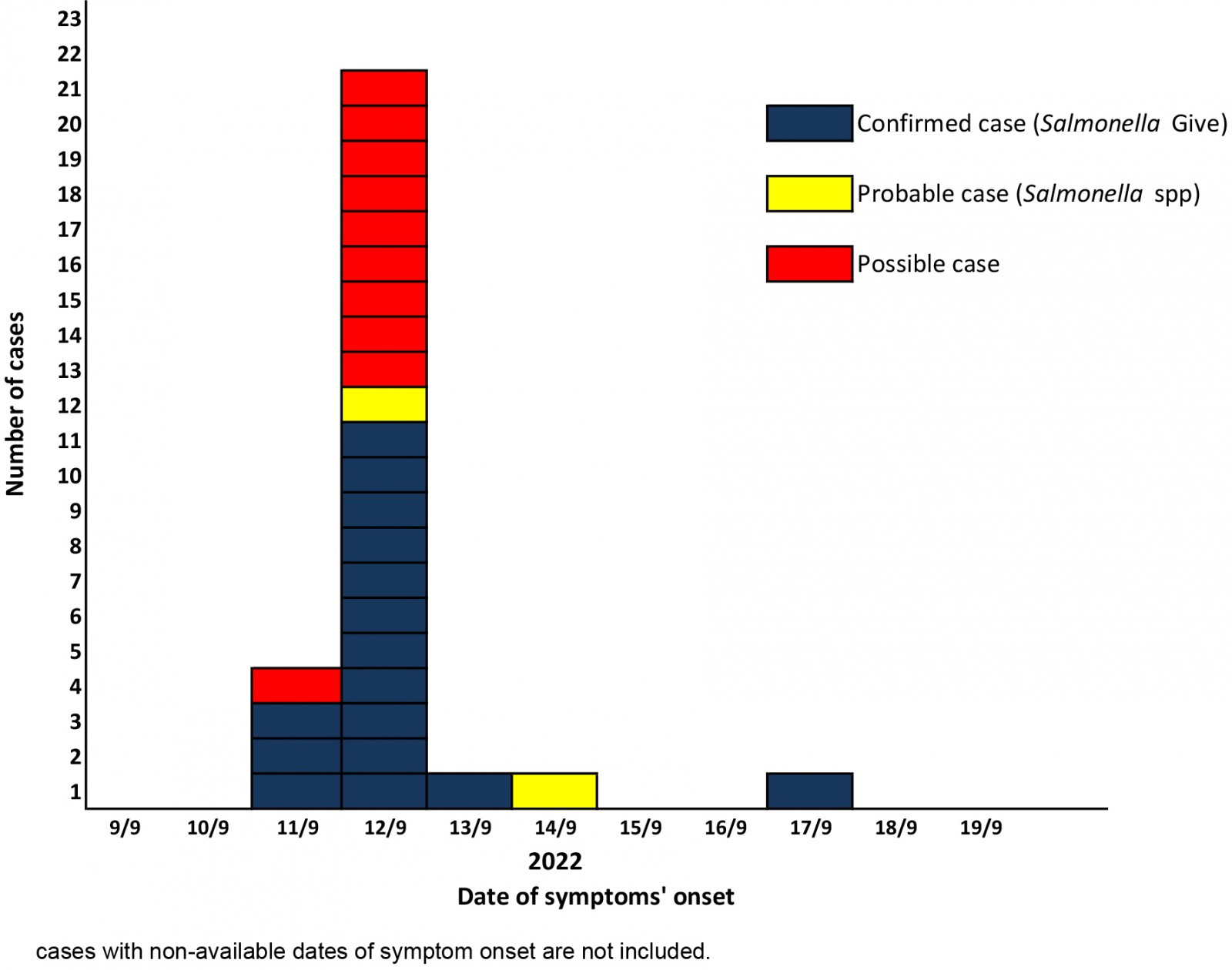 Figure 1: Number of confirmed, probable and possible non-typhoidal salmonellosis cases by date of symptom onset (n=28), local religious festival in region A in southern Greece, September 2022.†
Figure 1: Number of confirmed, probable and possible non-typhoidal salmonellosis cases by date of symptom onset (n=28), local religious festival in region A in southern Greece, September 2022.†
Laboratory investigation
All S. Give outbreak-associated food and human isolates and sporadic cases isolates implicated in salmonellosis cases in 2018 and 2022, in region A of southern Greece, presented a coincident antibiotype (all susceptible to the tested antimicrobial agents) and pulsed-field gel electrophoresis pattern. The two epidemiologically non-related S. Give isolates had a very different molecular profile (Fig2).
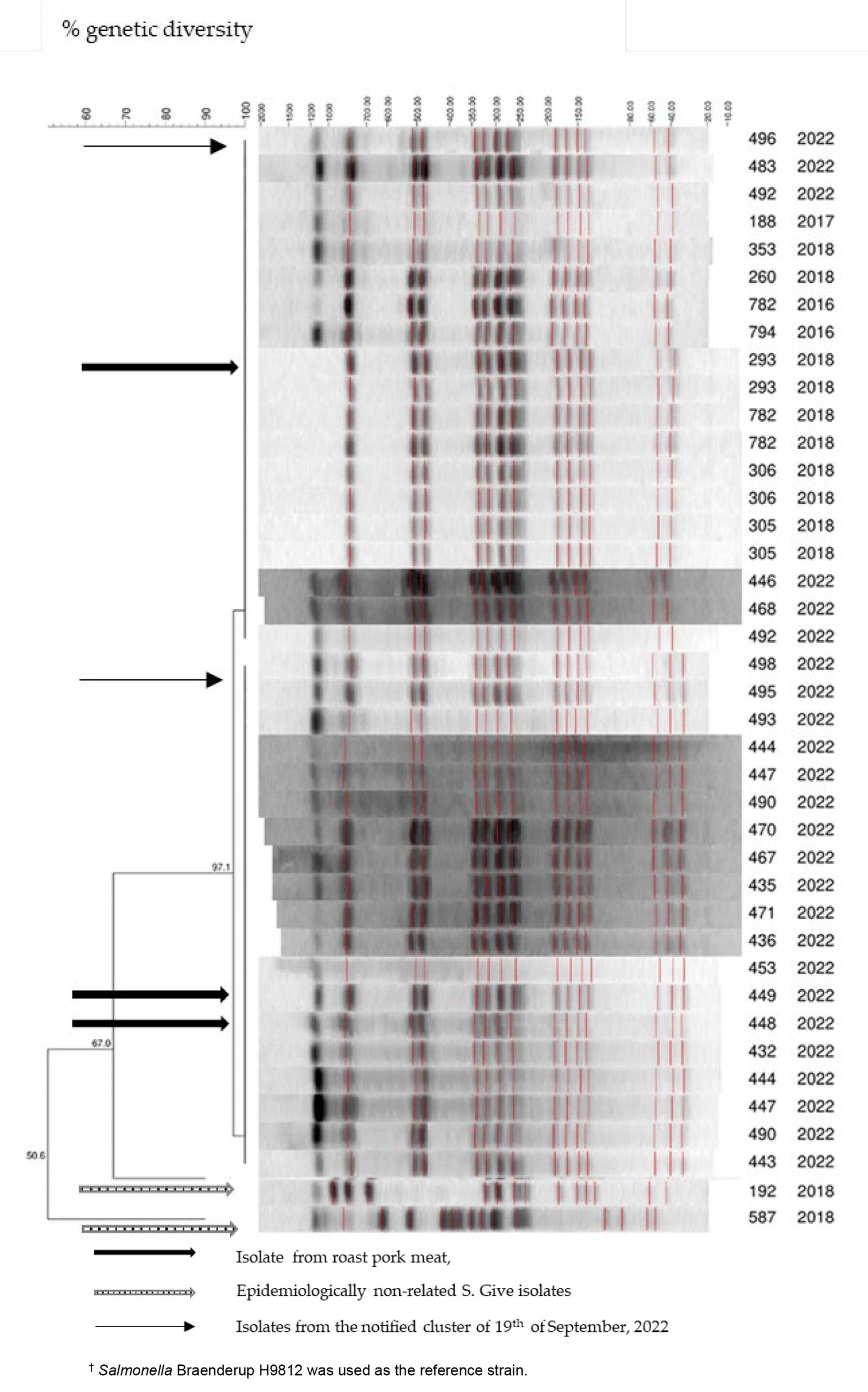 Figure 2: Pulsed-field gel electrophoresis profiles identified in human and food Salmonella isolates determined as S. Give, implicated in two outbreaks and in sporadic cases in 2018 and 2022, in region A, southern Greece.†
Figure 2: Pulsed-field gel electrophoresis profiles identified in human and food Salmonella isolates determined as S. Give, implicated in two outbreaks and in sporadic cases in 2018 and 2022, in region A, southern Greece.†
Environmental investigation
The food street vendor who sold the roasted pork meat at the local festival reported that he had bought the pig carcass whole from a supermarket in region A on 9 September 2022. On the same day, he transported it in his car to a region A bakery. On 11 September he transported the roasted pork meat, as well as the required food vending equipment, in the same car, to the festival to sell it to attendants.
The local public health authority and veterinary authority did not collect samples from the surfaces of the food vendor’s car and the equipment used, as they had been previously cleaned and disinfected by the vendor. A food traceback investigation was not feasible since information regarding the pork carcass batch was missing; no receipts or invoices were provided to the inspectors. The stool sample collected from the food vendor tested negative for Salmonella spp.
Additional information
On 19 September 2022, two non-typhoidal salmonellosis cases were reported via the Mandatory Notification System by a local general hospital of region A. Interviews with the medical doctors of the cases revealed that these patients, along with the other three members of the family, had consumed roasted pork meat; no other information was available. All five members of the family presented gastroenteritis symptoms; however, stool samples were collected by only two. Both Salmonella spp. isolates identified from the stool samples were sent to the Salmonella NRL and serotyped as S. Give. Communication with the cases was not feasible, therefore the roasted pork meat supplier could not be identified.
Public health measures
Public health measures were implemented, including suspension of roasted pork meat vending until the food street vendor was licensed by the competent authorities. In addition, information was provided to him regarding food safety practices. Enhancement of official inspections on food street vendors and on catering services of region A was recommended. Moreover, training on food safety principles and good hygiene practices of restaurant managers and all workers involved in the handling and processing of food, occupied in restaurants and catering establishments in region A, was strongly advised. Finally, strengthening of official controls in slaughterhouses within the framework of the application of Regulation (EC) 2073/2005, as well as strengthening the collection of sampling data for self-checks in slaughterhouses based on Reg. (EC) 2073/2005, were strongly suggested.
Discussion
Salmonella Give is a very rare serotype identified in humans in EU/EEA countries and Greece as well7,8,12. However, two S. Give outbreaks occurred during a 4-year period in a specific region of southern Greece that were epidemiologically linked to the consumption of roasted pork meat. Molecular typing by PFGE indicated that human and food Salmonella isolates of the 2018 and 2022 outbreaks belonged to the same S. Give strain.
The outbreaks occurred in a rural region of southern Greece, far away from the main town of the area, during local festivals, where the majority of participating visitors originated from different areas. The visitors returned the same day to their residences. As a result, cases visited many different healthcare facilities in different geographical regions. Thus, the determination of the extent of the outbreak and the communications with the directors of the abovementioned facilities, in the context of active case finding, proved to be complicated and time consuming.
The specific roasted pork meat recipe is a traditional one and it is very popular in region A, where the outbreaks occurred. It can be served either in restaurants or from food street vendors during mass-gathering festivals, which are frequently organized during summer months. Pig meat is among the five most common food vehicles with strong evidence of salmonellosis outbreaks7. However, according to the literature, S. Give has been implicated in only one pork meat-related outbreak in the past: in Germany, in 20049.
The high hospitalization rate of patients in the 2018 and 2022 outbreaks (40% and 57%, respectively), along with the notified median ages (16 years in the 2018 outbreak and 34 years in the 2022 outbreak) of hospitalized cases – which are not the usual high-risk age groups (<5 years old and elderly) – indicate a rather virulent S. Give strain. Similar findings have been reported in previous human S. Give outbreaks9-11.
Although traceback investigations in both outbreaks did not indicate the pig carcass or raw pork meat as the source of the pathogen, official and food business operator controls should be enhanced in order to early detect any deviations regarding breeding and slaughtering practices15.
Environmental investigations and inspections of the premises of restaurants, and the food street vendor involved, revealed significant deficiencies regarding food safety practices. The inadequate implementation of the Hazard Analysis Critical Control Point was one of the major findings in the investigation of the 2018 S. Give outbreak. The involvement of a food street vendor without any official certificates/licenses in transporting and selling a food item in high environmental temperatures is indicative of lack of compliance using minimum but fundamental hygiene measures. It should be noted that hygiene measures and official controls on food safety are less thorougly followed in rural areas where popular traditional festivals take place.
Implementation of appropriate food hygiene measures (eg handwashing, thorough cooking, safe storage conditions etc) assures food safety even when handling contaminated foodstuffs16. It should be noted that both S. Give outbreaks occurred during periods with high environmental temperatures in Greece, a condition that favors the growth of the pathogen when present in a foodstuff, raw or cooked17. The risk of a foodborne infection increases during summer periods due to higher temperatures and increased outdoor activities (private or mass). Therefore, food safety guidelines should be followed even more strictly, in order to minimize the risk of foodborne infections.
Outbreak investigations in Greece are conducted through collaboration between public health authorities, at central and regional levels, and public health and clinical laboratories18,19. Close cooperation among public health stakeholders is critical for timely and effective outbreak detection, response and intervention.
Conclusion
During investigation of a foodborne outbreak, limitations such as delays in the identification of the initial source or difficulties in the traceback investigation may emerge. Thus, cross-sectoral collaboration among human, environmental and animal health experts – in order to collect and share information to identify, investigate, control and when possible prevent the recurrence of a foodborne outbreak – is imperative. This collaboration is much more crucial when foodborne outbreaks occur in rural and remote areas. The One Health approach, which is a multisectoral and transdisciplinary collaboration among experts from the field of human, animal and environmental health and food safety, must be incorporated during a foodborne disease outbreak investigation in order to attain optimal health. Since Salmonella spp. is the most common zoonotic agent causing foodborne outbreaks, efforts to control and prevent salmonellosis should be enhanced in terms of stricter compliance to the control measures in the livestock industry and in mass or private food processing procedures. Food handlers must be trained and consumers must be systematically informed on hygiene practices that assure food safety. Food hygiene practices should be very thorougly followed in mass-gathering festivals (events that are very common in rural areas of Greece, mainly in summer months), where large quantities of local traditional recipes are prepared, handled, cooked and served to participants. Technical knowledge about pathogen transmission paths is important in order for both food handlers and consumers,to follow hygiene and sanitary measures. Efficient and enhanced official supervision, mainly during summer festivals, is required in order to avoid recurrence of foodborne infections by different combinations of pathogens/food commodities.
Funding
This research received no external funding.
Conflicts of interest
The authors declare no conflict of interest.
References
You might also be interested in:
2015 - Effect of rural practice observation on the anxiety of medical students

