Introduction
Working in the remote health sector can be incredibly rewarding, but also carries significant challenges1. The remote health sector in Australia experiences chronic understaffing and serves an isolated, culturally diverse population with a significantly higher burden of disease than metropolitan areas2. Despite the high health needs, remote health services struggle to recruit and retain enough skilled, dedicated staff to provide a stable service3. This is especially true in very remote primary health clinics, where small teams of remote area nurses (RANs), Aboriginal and Torres Strait Islander Health Practitioners (ATSIHPs) and Aboriginal Health Workers (AHWs) are responsible for providing or facilitating all health care for their local community4-6.
‘Remote area nurse’ is the term commonly used to describe registered nurses working in remote health centres/clinics without inpatient facilities7. RANs have an advanced-practice generalist role, delivering both acute and primary healthcare services to people of all ages7-9. Their responsibilities encompass diverse areas ranging from overseeing child health programs and managing chronic disease to handling medical emergencies and providing an emergency response in lieu of ambulance services1. To support RANs in effectively navigating this very broad scope of practice, various resources are available, including a voluntary credentialling process, short courses and postgraduate qualifications. Moreover, gaining hands-on experience in remote settings is seen as essential for attaining proficiency in the role1,7,9.
Poor personal safety has been identified as a contributing factor to burnout and high turnover of staff, and is linked to reduced quality of patient care10,11. For decades, poor WHS in remote clinics has been discussed in the literature as an issue in need of action12. As mentioned, in 2016 calls for change intensified following the murder of RAN Gayle Woodford13.
Many WHS recommendations and strategies have been developed for the remote health sector in Australia, such as a relevant orientation, education and training, a safe clinic building and accommodation, fit-for-purpose clinic vehicles, safe call-out processes and fatigue management5,14,15. However, there was very little evidence of the implementation of such safety strategies, despite many of these recommendations being made over a decade ago, followed by seemingly widespread agreement about their importance12.
Therefore, the aim of this study is to identify what WHS recommendations have been implemented in very remote primary health clinics within Australia, from the perspective of RANs. By asking RANs what specific WHS recommendations were in place in their clinics, this study attempts to quantify what safety strategies were actually in place, and where gaps existed.
Methods
Study design and population
This study used a cross-sectional survey to explore what WHS recommendations were in place, from the perspective of RANs from Australian very remote primary health clinics. The survey formed part of the lead author’s thesis, along with interviews with RANs and a WHS policy analysis16. This remote area safety project was designed in collaboration with a team of nurses with experience as RANs, educators, managers and researchers in different regions (see acknowledgements). The survey’s target population was all RANs who had worked in a very remote primary health clinic more recently than January 2019, classified as MM 7 (very remote) by the 2019 Modified Monash Model remoteness classification system17.
Data collection
The anonymous online survey was open to participants from December 2020 to January 2021. It was hosted on the Qualtrics survey platform (December 2020; https://www.qualtrics.com). A screening question was used at the beginning of the survey to ensure participants met the recency of RAN practice and remoteness inclusion criteria. The information and consent page detailed the survey’s purpose, confidential use of information, ethics approval, researcher contact details, and psychological support details. The full questionnaire is published in Appendix 2 of the lead author’s thesis16. Participants were recruited using convenience sampling as RANs are a geographically dispersed, hard-to-reach population. Professional networks were used to advertise the survey, including the member communications and newsletter of CRANAplus (the peak body for remote health professionals in Australia), Australian College of Nursing communications to their rural nursing community of interest, RAN Facebook groups, and word of mouth.
Although the total population of RANs at the time of the study was unknown, it was estimated that 825 RANs would be eligible to participate based on the number of RAN positions in 2008 and the turnover rates for 2013–20153,18. Therefore, approximately 21% (n=173) of the target population completed the survey. The minimum acceptable sample size for this survey was 96 participants, based on a 95% confidence interval (Z), 50% expected proportion (p), and 10% precision (d): n = Z2p(1 – p)/d2 19. The sample size achieved gives a precision of 7.5% or better.
The questionnaire was developed by the project team, which included several experienced RANs. A combination of validated tools and remote-specific workplace safety recommendations were used to ensure the questionnaire would be relevant to RANs from all regions and remote clinic types within Australia. The questionnaire predominantly included multiple-choice questions about which safety strategies were in place in participants’ current or most recent very remote primary health clinic. Additional information was gathered with Likert/ranking scales and free-text comments.
Data analysis
A score to quantify the safety of RANs’ workplaces was calculated using 55 detailed workplace safety recommendations derived from previous literature. All 55 recommendations were included in the survey, with one point awarded per recommendation met. The workplace safety score focuses on preventative measures, so incident rates and downstream interventions such as post-incident support are not included in this article, but are explored in the lead author’s thesis16. For ease of interpretation, the score is presented as a percentage of recommendations met.
Descriptive statistics were used to present the workplace safety score and rates for the individual recommendations. Results were presented as means for normally distributed data, or as medians for data that weren’t normally distributed. N indicates the overall total sample, and n denotes the subsample. When assessing variation in safety scores, independent samples t-tests, Kruskal–Wallis tests and Mann–Whitney U-tests were used. Table 1 provides further detail.
We also explored the variation in safety scores between various workplace characteristics. When overall safety scores were compared by state/territory, the Indian Ocean Territory data (n=1) were combined with those of Western Australia. As New South Wales and Victoria had few participants and their scores were similar, their data were combined. When assessing the relationship between clinic size and safety, clinic staffing was used as an indicator of clinic size.
Table 1: Data analysis methods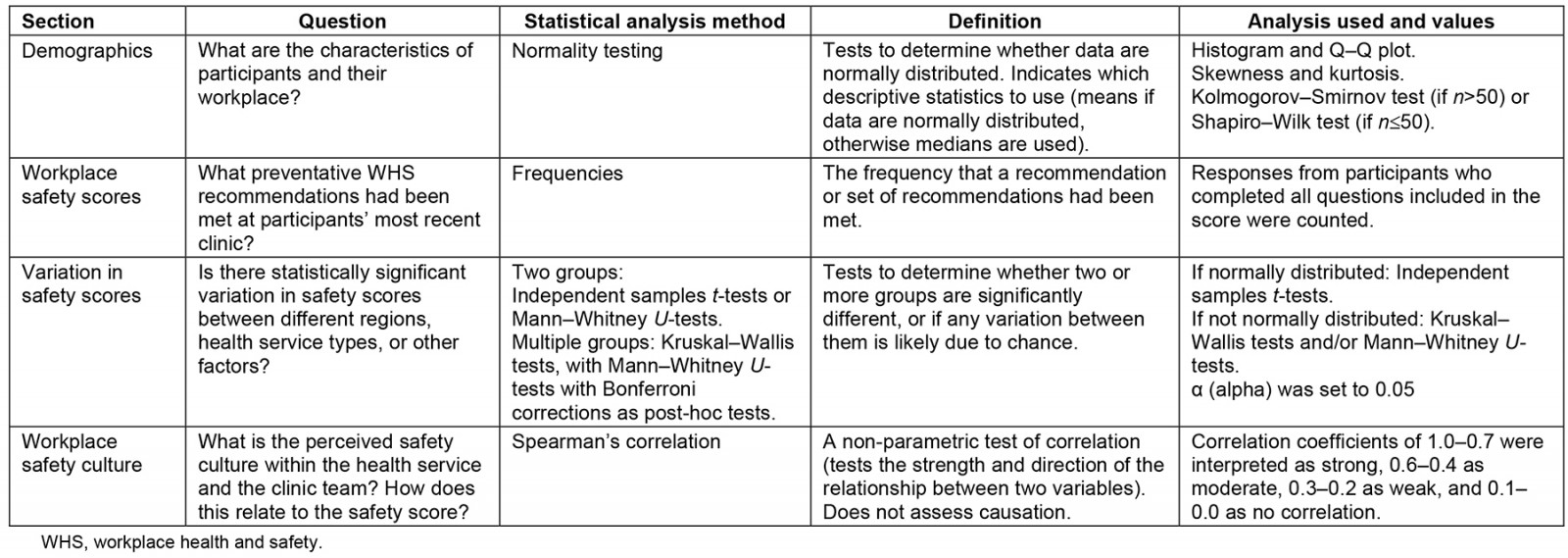
Ethics approval
This study was conducted in accordance with the National Statement on Ethical Conduct in Human Research20. Ethics approval was granted by the James Cook University Human Research Ethics Committee (application ID H8255).
Results
Respondent characteristics
Table 2 shows the demographics of the 173 RANs who completed the survey. Respondents’ median age was 56 years (interquartile range (IQR) 13), 146 (84.4%) were female, 114 (65.9%) had postgraduate qualifications, 170 (98.3%) were non-Indigenous, 134 (77.5%) were born in Australia and 91 (52.6%) grew up in a rural or remote area. The RANs commonly worked away from their families, as 109 (63%) participants had a partner, but only 42 (38.5%) of those partners lived in the remote community with the RANs. The participants had a median 7 years of RAN experience and had been working a median 12 months at their current workplace. Thirty six participants (20.8%) were clinic managers.
The Northern Territory had the highest proportion of participants, with 92 (53.2%), followed by Queensland’s 35 participants (20.2%) and Western Australia’s 31 participants (17.9%). Ninety-nine (57.2%) worked for a government-run health service, 53 (30.6%) were employed by an agency and 76 (43.9%) were on locum or similar short-term contracts.
Table 3 shows the number of RANs and Aboriginal or Torres Strait Islander Health Practitioners/Health Workers (ATSIHPs/AHWs) employed at each clinic. Most participants worked in small clinics: 48 (27.9%) had two RANs and 33 (19.2%) had three RANs. Some clinics were much larger, with 22 participants (12.8%) working in clinics with eight or more RANs. Single-nurse posts were not fully phased out: 17 participants (9.9%) were the only RAN at their clinic. Notably, 58 participants (34.3%) reported there were no ATSIHPs or AHWs currently employed at their workplace. No data were collected on the number of vacant positions.
Table 2: Respondent demographics (N=173)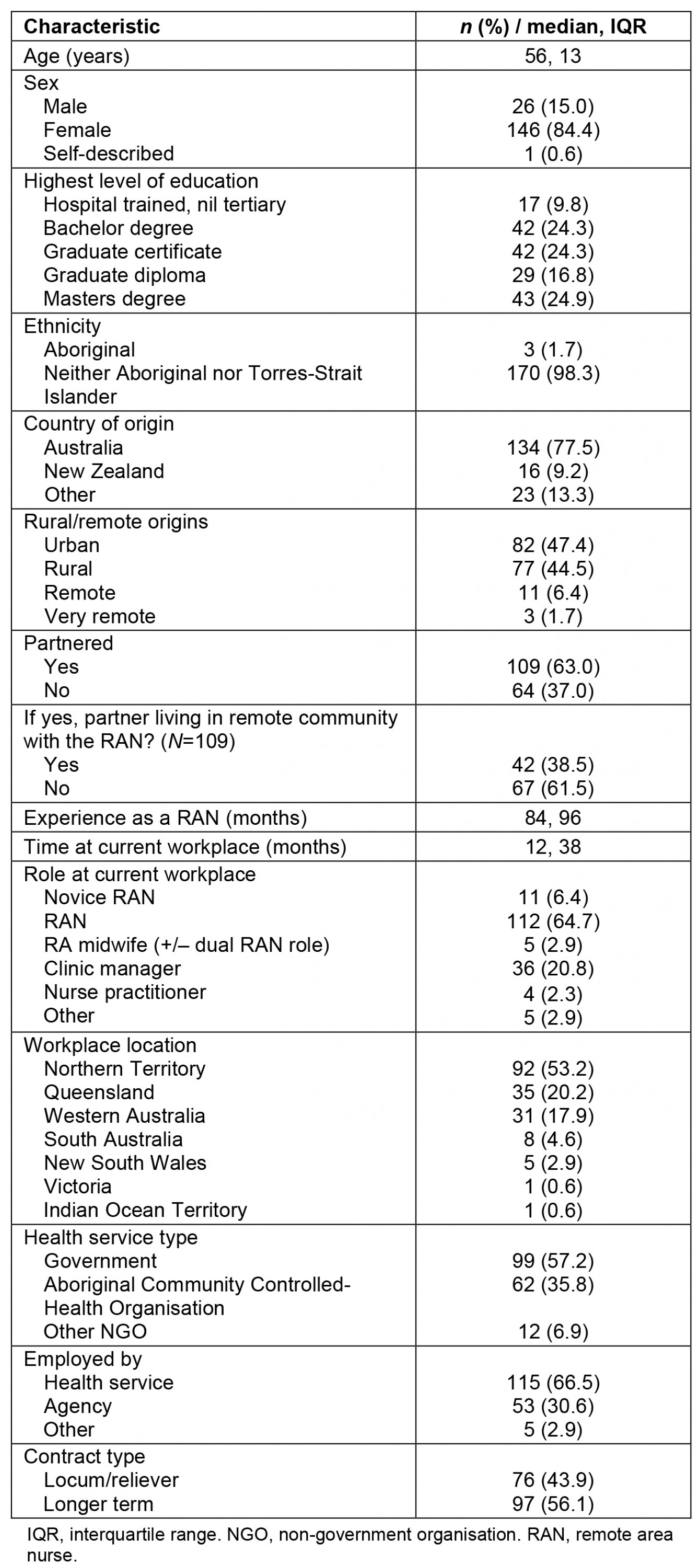
Table 3: Number of RANs (N=172) and ATSIHPs/AHWs (N=169) employed at participants’ workplaces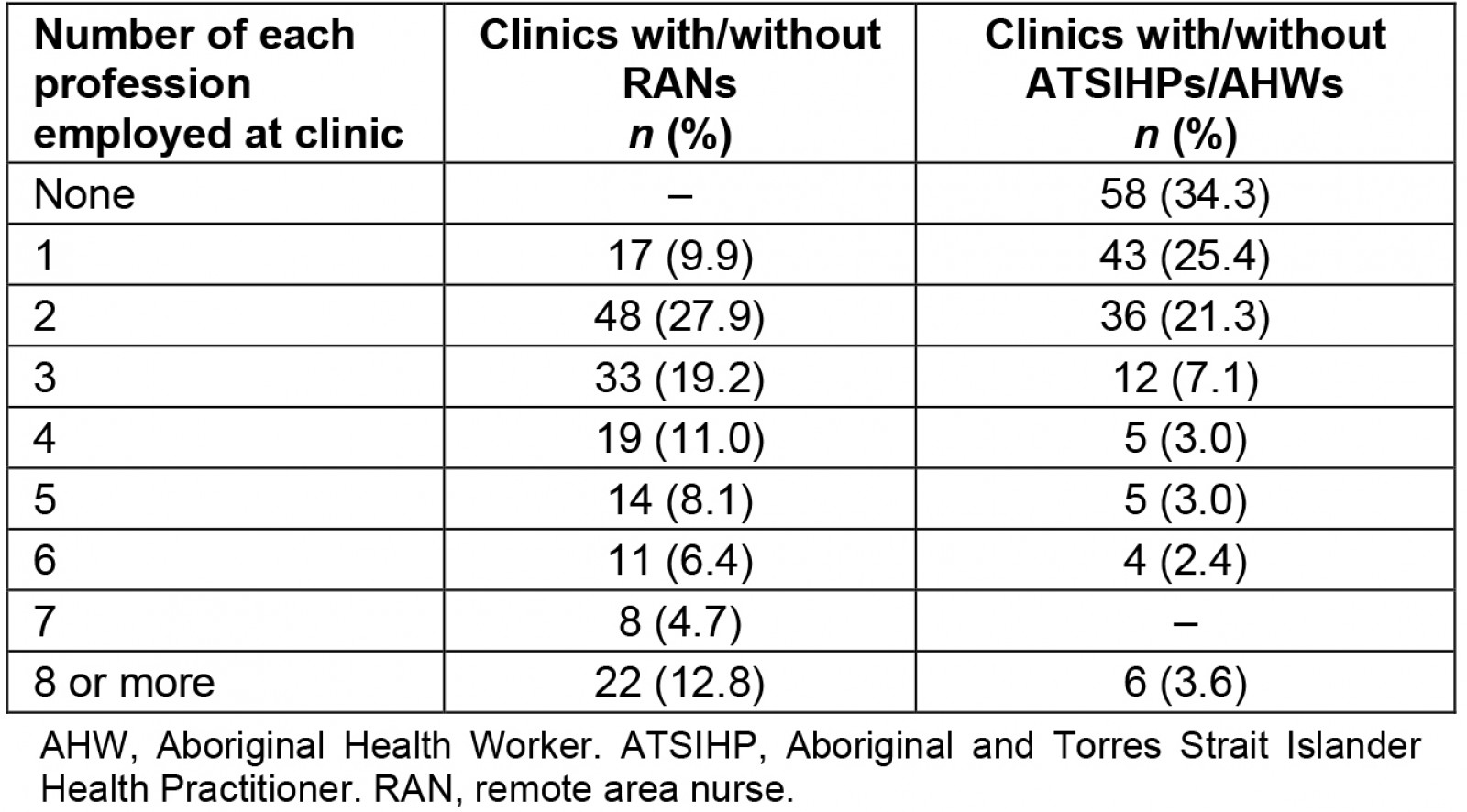
Workplace safety scores
Workplace safety scores show the proportion of preventative WHS recommendations that were implemented in very remote primary health clinics across Australia. An overview of the national scores is pictured in Figure 1. On average, 53.1% (SD 19.8%) of the WHS recommendations had been met. This can be divided into three broad domains: staff preparation (orientation, training and the provision of safety policy information), safe work environment (clinic, accommodation and vehicle safety) and safe work practices (‘never alone’ and other call-out safety strategies, and fatigue management). Staff preparation scored 38.5% (IQR 46.2%), safe work environment scored 59.4% (IQR 34.4%) and safe work practices scored 50.0% (IQR 36.7%).
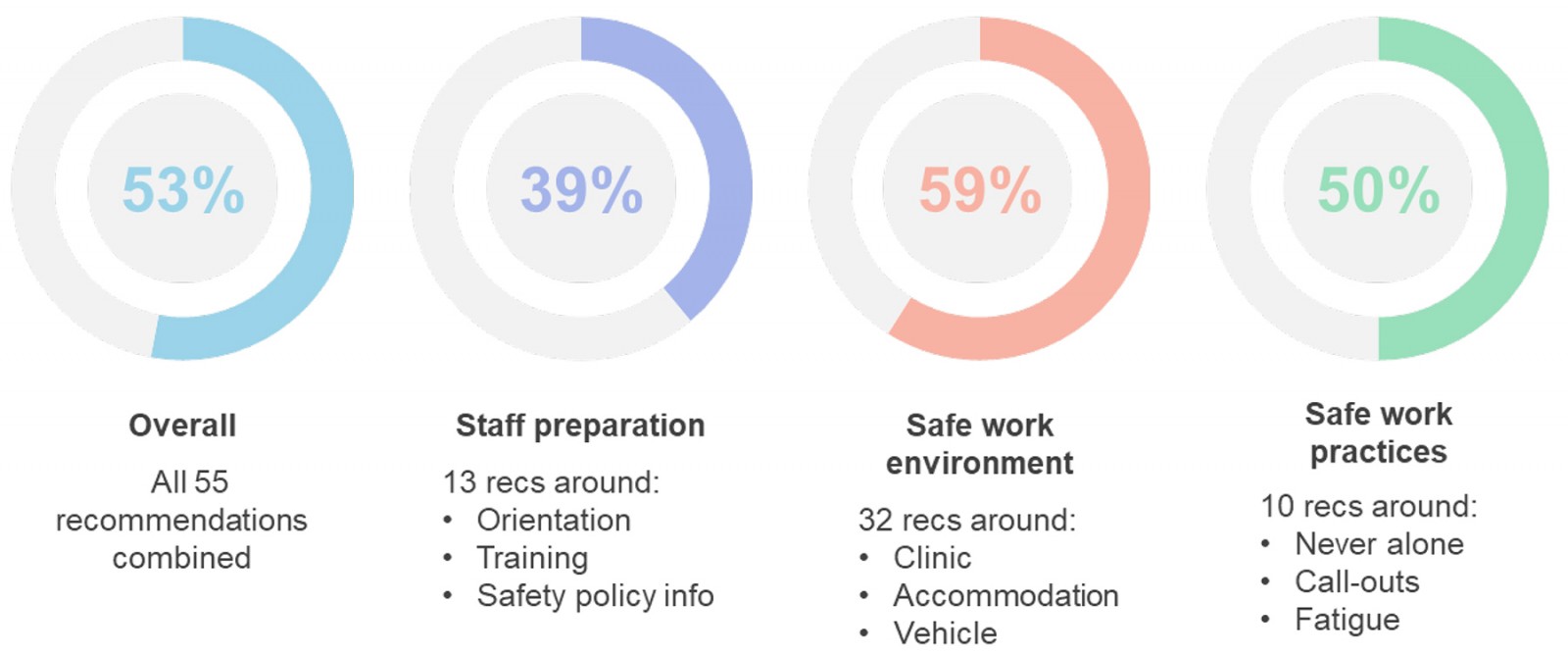 Figure 1: Percentage of workplace health and safety recommendations met for very remote primary health clinics in Australia.
Figure 1: Percentage of workplace health and safety recommendations met for very remote primary health clinics in Australia.
Staff preparation domain: Staff preparation scored the lowest of the three domains, representing the orientation and training of RANs to help them fulfil their role safely. Local orientation only scored a median of 33.3% (IQR 83.3%) of recommendations met. Low rates of orientation were the main driver of this low score, as 30.6% (57/186) of participants did not receive any local orientation on commencement at their workplace. Table 4 details what safety topics were included where participants received an orientation.
Information on safety related policy and procedures was received by 57.0% (106/186) of participants before they started work.
Safety training also only scored a median of 33.3% of recommendations met (IQR 50%) (see Table 5).
Table 4: Safety topics reported by RAN study participants as being included in orientation and training (N=119)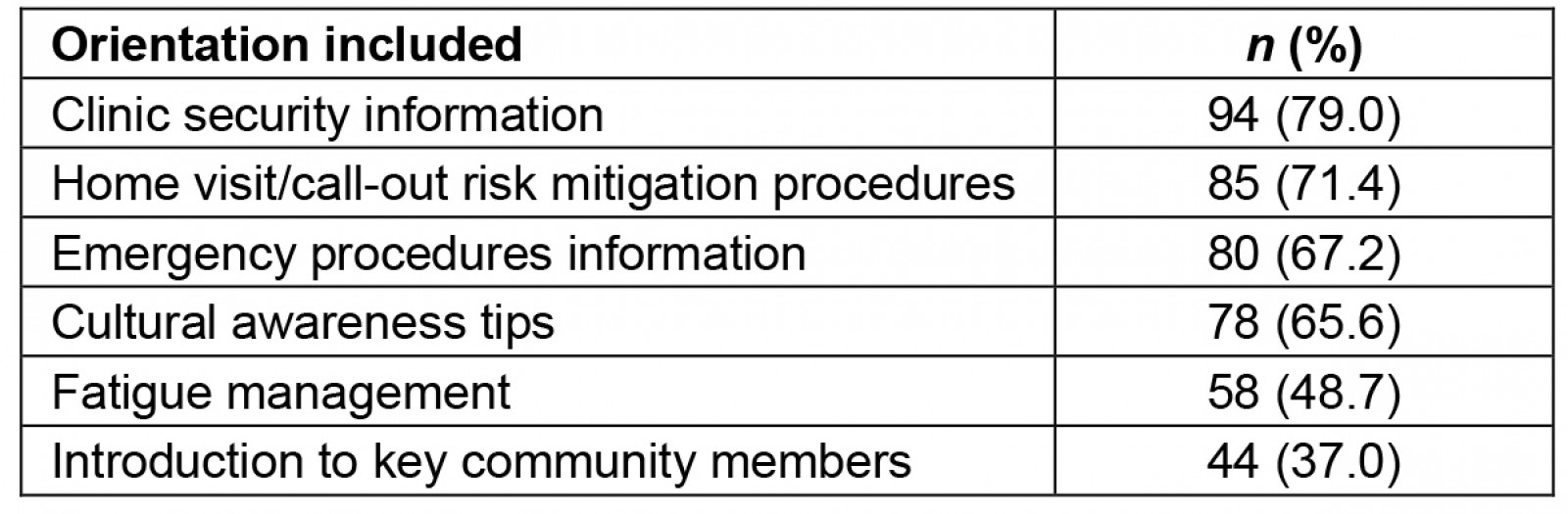
Table 5: Safety training reported by RAN study participants as being included in orientation and training (N=173)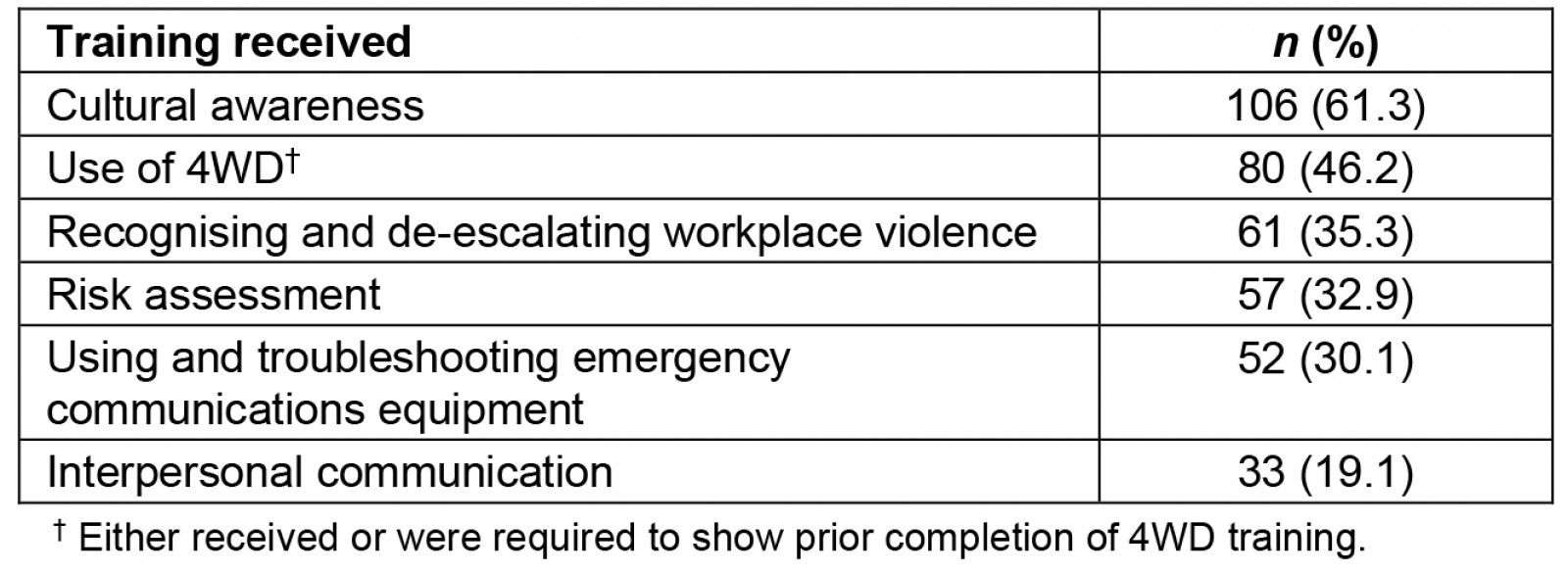
Safe work environment domain: The safe work environment domain includes clinic safety and security, clinic vehicle safety and accommodation safety. With a median score of 59.4% (IQR 34.4%), this domain had the most recommendations met.
Clinic safety scored highest within the domain, with median 70.0% (IQR 40.0%) of recommendations met. As shown in Table 6, basic safety features were fairly common in participants’ clinics, such as having more than one exit, good lighting at external entry points, and effective locks on all external doors. However, maintenance was highlighted as an issue, with only 61.6% (106/172) of participants claiming their clinic buildings were well maintained.
Clinic security scored lowest within the domain, with median 40.0% (IQR 40.0%) of clinic security recommendations met. While a majority of participants had duress alarms/panic buttons in their workplace, other security technologies and processes were relatively uncommon (see Table 7).
Clinic vehicle safety scored a median of 60.0% (IQR 40.0%). Most clinic vehicles were fitted with a basic tool kit (at minimum, a jack and wheel brace), but maintenance was again identified as an issue, with only 56.4% (97/172) of participants reporting their clinic vehicle was reliable and adequately serviced. Although the individual rates were low for vehicle-based communications technologies (see Table 8), 72.7% (125/172) of participants report their clinic vehicle had at least one of the three technologies (a satellite phone, GPS tracking or a personal locator beacon).
Staff accommodation safety scored a median of 66.7% (IQR 41.7%). Similarly to the clinics, the most basic safety features were commonly met in staff accommodation, such as working curtains/coverings for the windows, effective locks on the external doors and working fire alarms (see Table 9). Examples of less commonly implemented strategies include good maintenance, a reliable phone/telecommunications service and good lighting where the vehicle is parked.
Separate from the workplace safety score questions, participants also rated how well maintenance was done at their workplace, on a scale of 1 to 10. Maintenance of staff accommodation was rated a median of 3 (meaning ‘significant delays in repairs’, IQR 3–5). The remaining areas were rated a median of 5 (meaning ‘maintenance requests actioned’), including maintenance of the clinic building (IQR 3–5), clinical equipment (IQR 3–5), clinic vehicles (IQR 3–7), and alarms/communications technology (IQR 3–6). For staff accommodation, 13.7% (23/168) of participants said maintenance requests were ignored. For clinic vehicles, there was an effective proactive maintenance schedule for 11.9% (20/168).
Table 6: Clinic safety as reported by RAN study participants (N=172)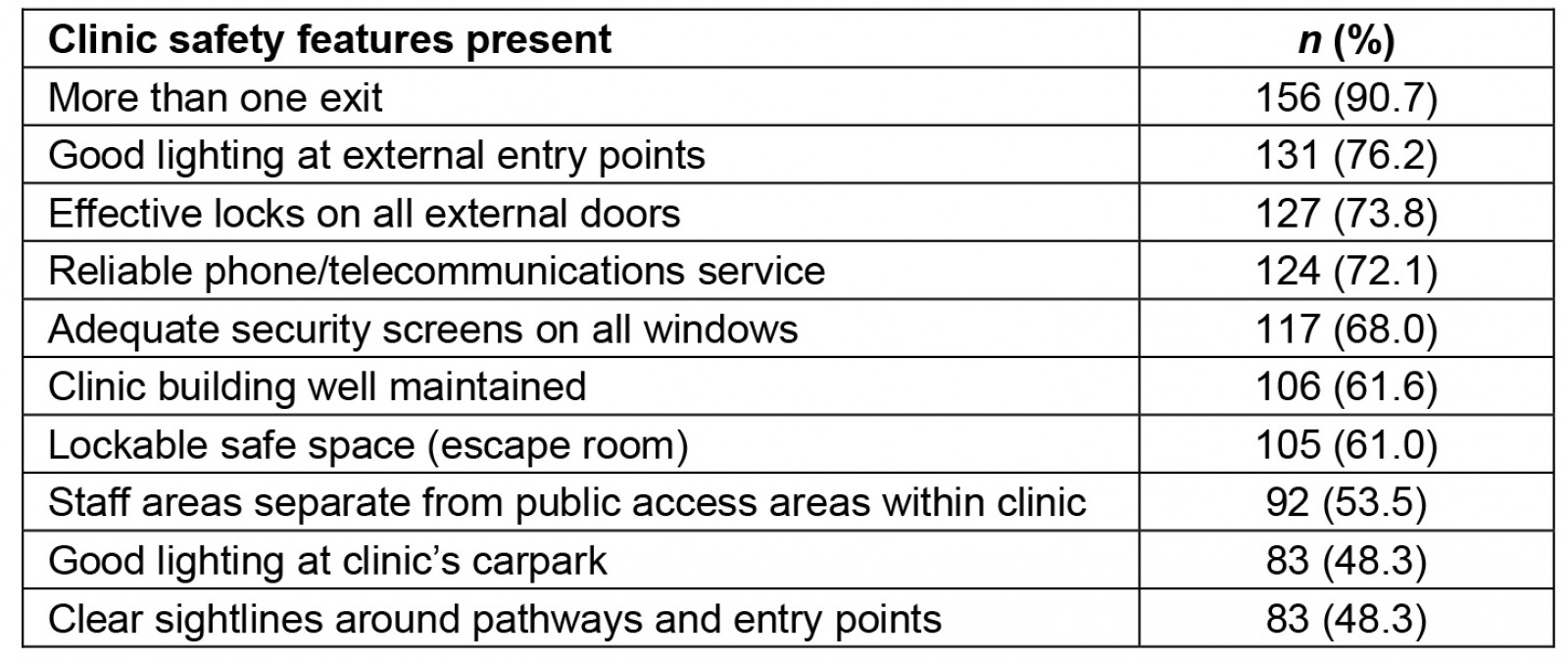
Table 7: Clinic security as reported by RAN study participants (N=170)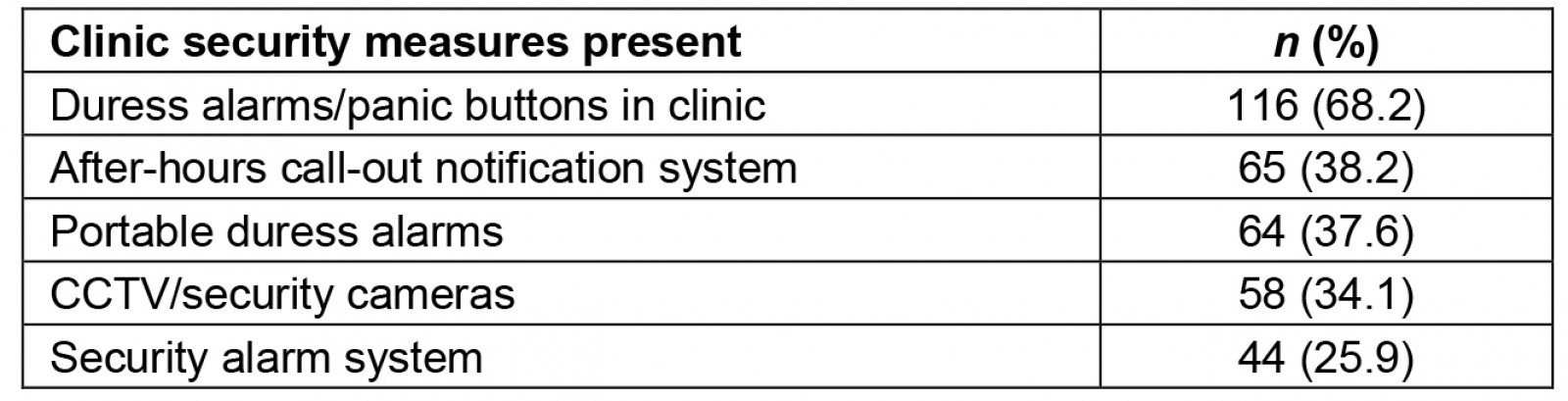
Table 8: Clinic vehicle safety as reported by RAN study participants (N=173)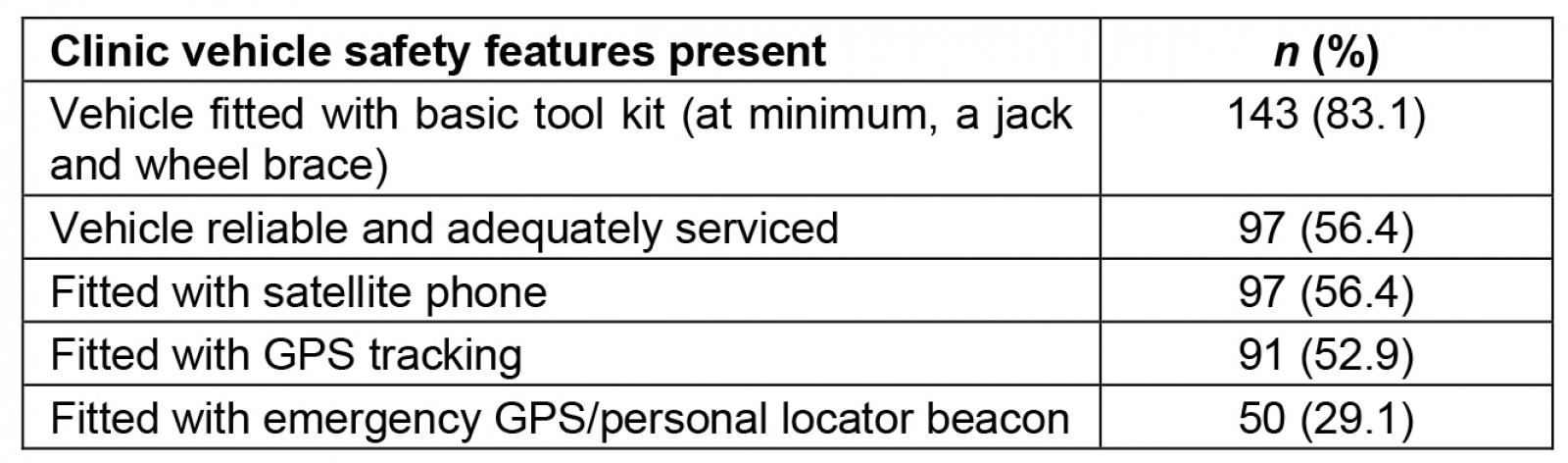
Table 9: Staff accommodation safety as reported by RAN study participants (N=173)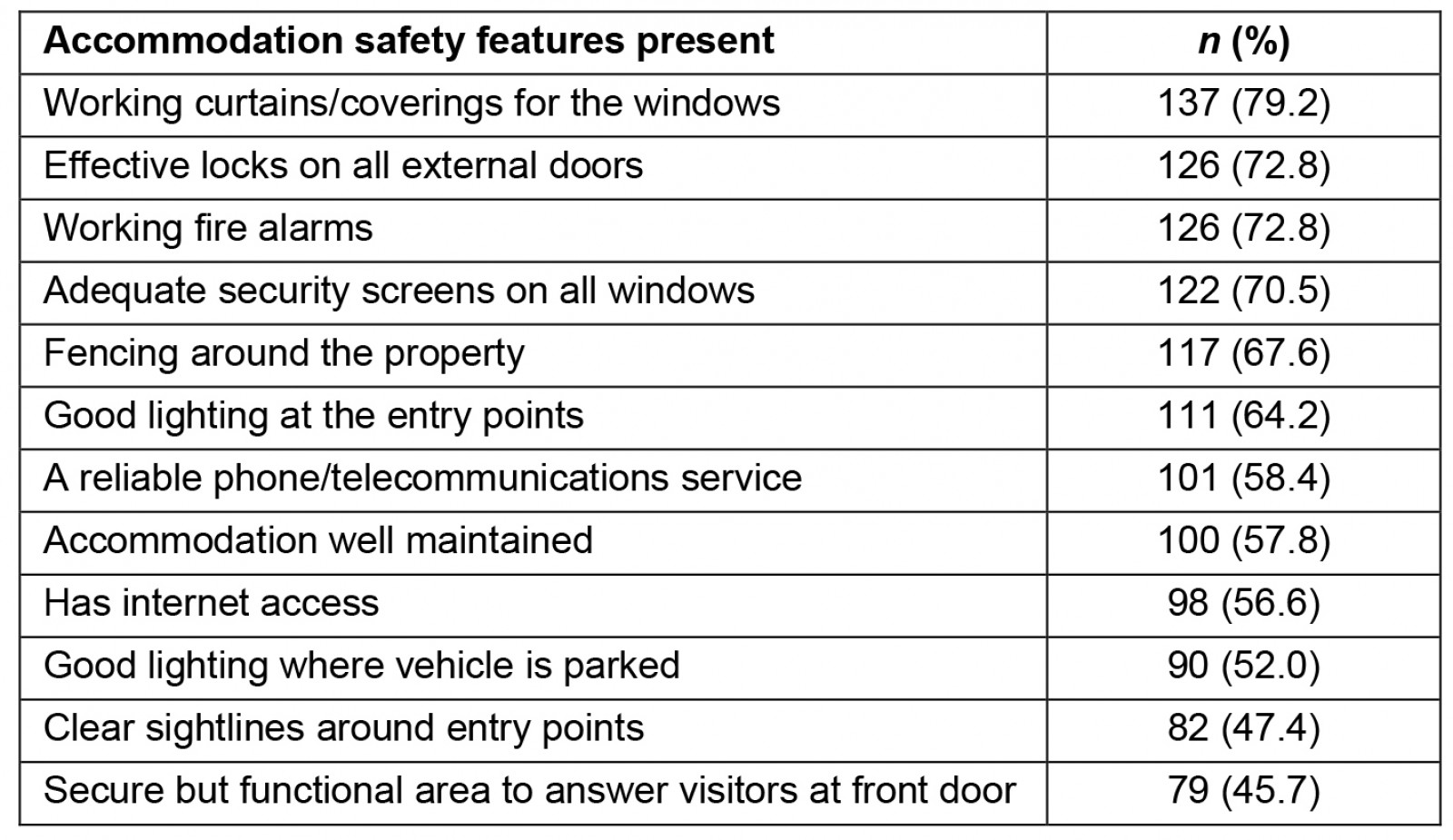
Safe work practices domain: The safe work practices domain scored median 50% (IQR 36.7%) of recommendations met, covering call-out/home visit safety and fatigue management. Table 10 details the rates for individual safety strategies in this domain.
Second responders were required for all home visits and call-outs for 49.7% (83/167) of participants, and a further 14.4% (24/167) were required to have a second responder for all call-outs but not home visits. Where ‘never alone’ policies were in place, participants reported that most managers and RANs consistently supported and implemented the policy. Managers were seen to show slightly higher support for the ‘never alone’ policy than the RANs did.
Call-out systems that discouraged patients/clients from attending staff accommodation to seek treatment were in place for 81.1% (129/159) of participants.
Fatigue management scored a median of 40.0% (IQR 40.0%). Having a fatigue management policy/protocol and protected rest hours after overnight call-outs were in place for a slim majority of participants, but less than a third had adequate staffing/skill mix to share on-call responsibilities or the ability to take scheduled leave regularly.
Many participants added free-text comments about fatigue management in their workplace. Four described the undermining of fatigue management policies: ‘Unfortunately this is often either ignored or staff are 'encouraged' to reduce their fatigue hours’ (participant 16). Five participants negotiated fatigue leave with their manager on a case-by-case basis, while two participants from single-nurse posts were unable to take fatigue leave without closing the clinic. Three participants wrote of organisational disinterest in fatigue management, for example, ‘Have been told fatigue management is my responsibility’ (participant 94). Two participants wrote about how COVID-19 exacerbated fatigue management issues, for example, ‘Due to Covid, I have only had one week's annual leave all year but usually I would ensure I take annual leave every 4–5 months’ (participant 93).
Table 10: Safe work practices as reported by RAN study participants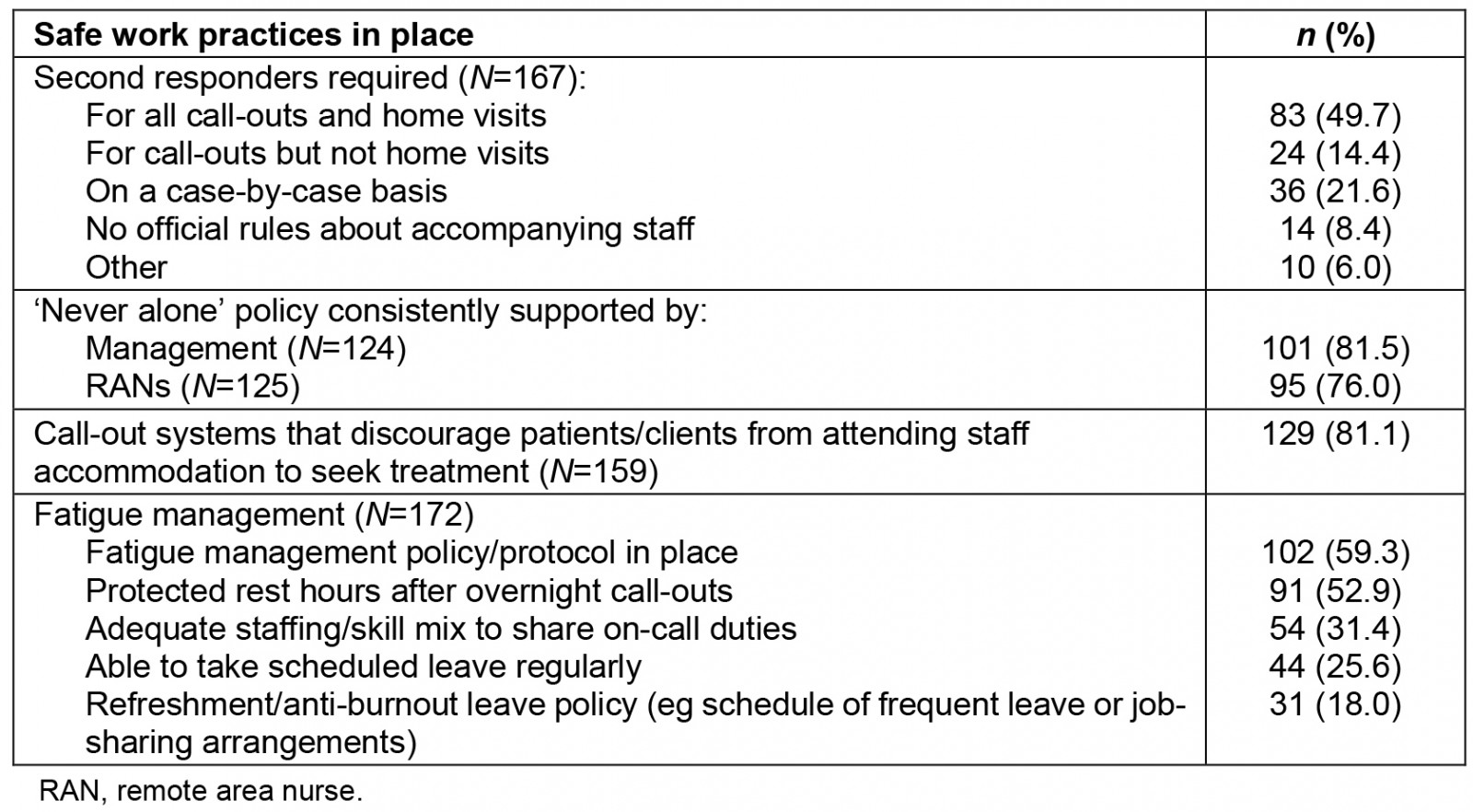
Variation in safety scores
State/territory: Average overall workplace safety scores by state/territory are presented in Figure 2 and Table 11. Significant variation in those scores was found between the Northern Territory (57.5%, standard deviation (SD) 18.7) and Queensland (41.7%, SD 16.7%) (p<0.01), and between South Australia (74.5%, IQR 35.9%) and Queensland (p<0.05). This variation also holds true for the individual domains:
- Within the staff preparation domain, significant variation was found between the Northern Territory (46.2%, IQR 44.2%) and Queensland (23.1%, IQR 30.8%) (p<0.05), and between South Australia (69.2%, IQR 44.2%) and Queensland (p<0.05).
- Within the safe work environment domain, significant variation was found between the Northern Territory (65.6%, IQR 31.3%) and Queensland (47.9%, SD 20.3%) (p<0.01).
- Within the safe work practices domain, significant variation was found between the Northern Territory (60.0%, IQR 30.0%) and Queensland (35.0%, IQR 50.0%) (p<0.01), South Australia (80.0%, IQR 40.0%) and Queensland (p<0.01), and Western Australia (43.0%, SD 24.0%) and South Australia (p=0.01).
Table 11: Percentage of workplace health and safety recommendations met for very remote primary health clinics, by state/territory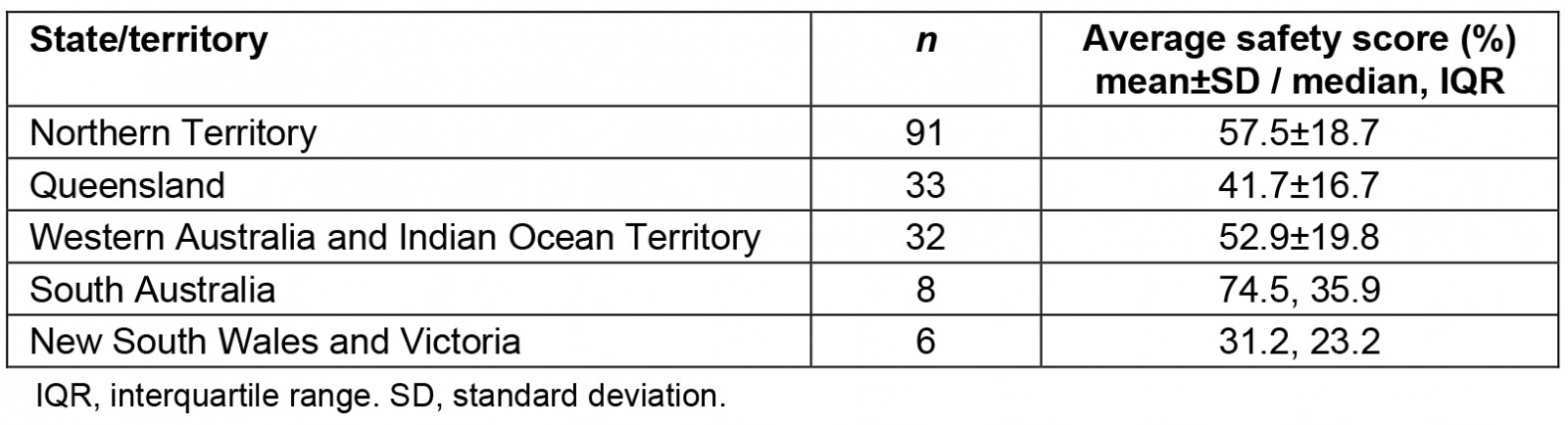
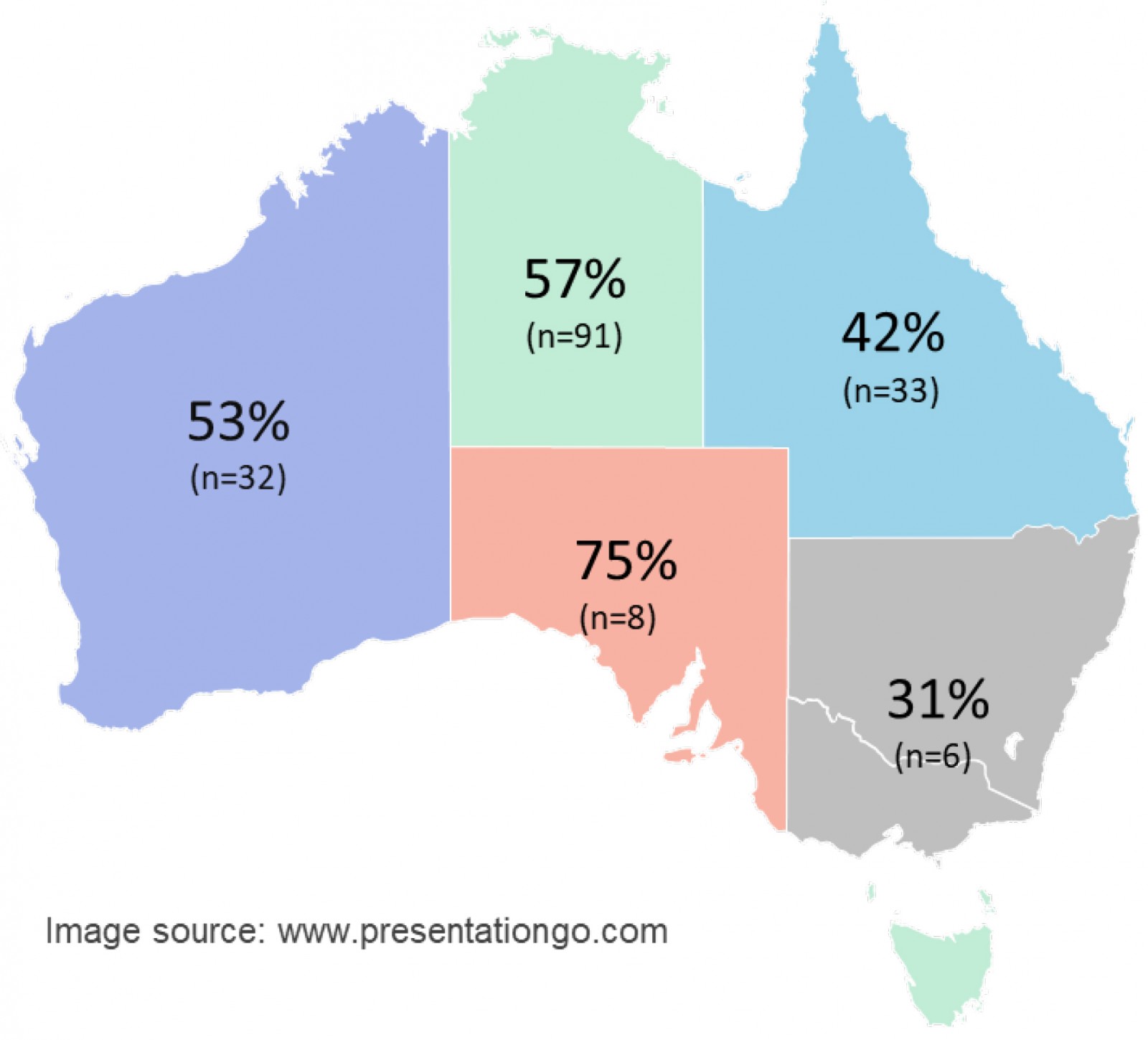 Figure 2: Percentage of workplace health and safety recommendations met for very remote primary health clinics, by state/territory21.
Figure 2: Percentage of workplace health and safety recommendations met for very remote primary health clinics, by state/territory21.
Health service type: Nationally, there was no statistically significant difference in the mean safety scores between government-run clinics (52.9%, SD 19.7%), clinics run by an Aboriginal Community Controlled Health Organisation (ACCHO) (53.1%, SD 19.5%), and clinics run by other non-government organisations (63.6%, IQR 43.6%).
When split by state/territory, a significant difference in safety scores was found in the Northern Territory between government-run clinics (62.0%, SD 16.8%) and ACCHO-run clinics (49.9%, SD 19.1%) (p<0.01). There was no significant difference between service types in Western Australia. Sample sizes in other regions were insufficient to compare by service type, but it is notable that almost all Queensland participants (31/33) worked in government-run clinics, with an average safety score of 42.4% (SD 16.6%), and most South Australian participants (6/8) worked in ACCHO-run clinics, with a median safety score of 77.3% (IQR 16.4%).
Other clinic factors: For clinic size, no correlation was found between the number of RANs or ATSIHPs/AHWs employed at a clinic and that workplace’s safety score.
For staffing type, there were no significant differences between the workplace safety scores of locum (52.7%, IQR 33.2%) and longer term staff’s clinics (52.8%, SD 19.7%), or between the workplaces of RANs employed by a health service (53.6%, SD 20.3%) or an agency (53.3%, SD 19.0%). Additionally, no statistically significant differences in the median staff preparation domain scores were found when comparing locum (38.5%, IQR 50%) and longer term (30.8%, IQR 46.2%) staff, or between staff employed by a health service (38.5%, IQR 53.8%) or an agency (38.5%, IQR 38.5%).
Workplace safety culture
Participants’ perceptions of the safety culture within their health service and within their clinic team were measured on a scale of 1 (‘terrible’) to 10 (‘excellent’). The median perceived safety culture was 6/10 (IQR 4) within the health service and 8/10 (IQR 3) within the clinic teams. When divided by state/territory, the clinic team was perceived to have a stronger safety culture than the health service everywhere except South Australia (see Table 12).
There was a moderate positive correlation between the perceived workplace safety culture within health services and workplaces’ safety scores (rs=0.633, n=151, p<0.01), and a weak positive correlation between the perceived safety culture within clinic teams and workplaces’ safety scores (rs=0.333, n=150, p<0.01).
Table 12: Perceived workplace safety culture by state/territory (scale of 1–10†)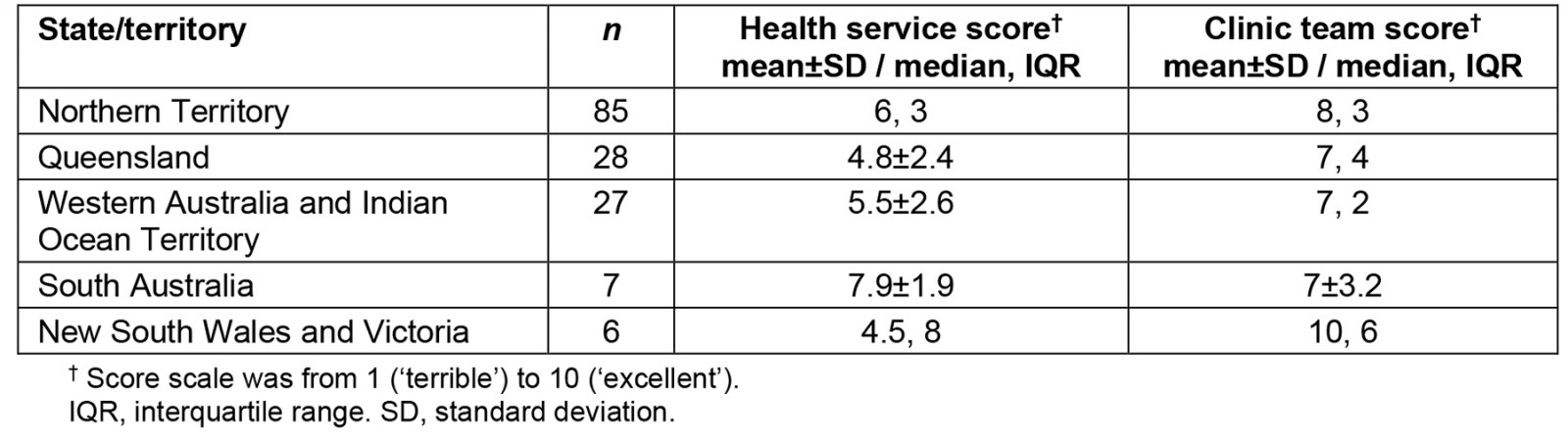
Discussion
This survey illustrated the current state of workplace safety in primary health clinics within very remote Australia. Major gaps were found in the implementation of recommended safety strategies, with significant regional variation in the extent of implementation.
In Australia, the regulation of WHS in remote health falls under the Work Health and Safety (National Uniform Legislation) Act 2011 and Regulations, exhibiting minor variations across jurisdictions22. However, this study showed persistent regional variation in the implementation of preventative WHS measures. In South Australia, the divergence can be explained, in part, by the recently introduced Health Practitioner Regulation National Law (South Australia) (Remote Area Attendance) Amendment Act 2017 and its accompanying regulations, commonly known as ‘Gayle’s law’. This Act mandated that health professionals in remote areas of South Australia must be accompanied by a second responder for all after-hours or unscheduled call-outs.
South Australia’s increased focus on WHS seems to extend to staff preparedness, as South Australia also had the highest safety score in that domain. However, it is noteworthy that this may be indicative of how poorly orientation was done in other states, as evidenced by the findings of the Gayle’s Law Review conducted at the same time as this study. The review identified that only 57% of remote health practitioners in South Australia had participated in an organisational orientation program13. A robust local orientation process is crucial for improving staff safety and quality of patient care5,23. While this survey indicates an improvement, with 69% of RANs receiving orientation on commencement compared to 50% in 2017, there are significant gaps in the content of the orientation provided4.
Many participants did not receive information for developing good relationships with the community, such as local cultural safety training, which is a valuable foundation for cultivating culturally safe practice24. The National Rural and Remote Nursing Generalist Framework identifies culturally safe practice as the central domain that wraps around all other practice areas8. The cultural competence of RANs significantly influences community members’ willingness to use a clinic, carrying significant implications for primary health care25. Poor cultural safety also hampers the functioning of the clinic team, as Dunbar et al found that RANs often display only superficial respect for ATSIHPs, with few examples of two-way learning25. Given the lack of cultural safety training and the fact that 34% of participants didn’t have ATSIHPs or AHWs at their workplace, there is much room for improvement in cultural safety.
Training in safety skills was highly recommended in the literature12, especially training in recognising and managing workplace violence4,6,23,26. However, training in workplace violence prevention was much less common for RANs in this survey compared to those in previous surveys of rural/remote health professionals, with 35% in the current survey, 45% in 201211, and 67% in 200827. While not directly comparable (all three studies used different rural/remote selection criteria), the ongoing low rates of training combine with the orientation gaps to suggest the RAN workforce had not received adequate preparation for their role.
This study also found that poor fatigue management was very common for RANs. Safe Work Australia defines fatigue in a work context as ‘a state of mental and/or physical exhaustion which reduces a person’s ability to perform work safely and effectively’28. Poor fatigue management for healthcare workers directly impacts staff health29, can reduce the quality of patient care and is a barrier to staff recognising and constructively managing the warning signs for workplace violence15. This highlights the need for a widespread culture shift around fatigue management in the remote health sector.
Another concern was the proportion of RANs living in unsecure housing, despite this being identified as a high-risk location for workplace violence4. For example, one in four participants did not have effective locks or working fire alarms in their accommodation. Other safety features were even less common, despite safe staff accommodation being a specific requirement in the WHS (National Uniform Legislation) Act 2011. Other common infrastructure-type hazards identified in this study are covered in the WHS (National Uniform Legislation) Act 2011 and Regulations, while the Managing the Work Environment and Facilities Code of Practice provides specific examples of how to resolve those hazards30. In addition to this legislation, repeated studies over the decades have identified the same WHS issues faced by RANs, with similar recommendations provided to address them12. Despite this, the WHS issues persist, as shown by the current study. Legislation alone is not enough to address these issues in remote health settings.
We recommend that a multi-level, multi-faceted approach is taken to create meaningful and sustainable change in the remote health sector’s approach to WHS. To achieve this, WHS performance indicators should be embedded within health services’ quality improvement processes, including the development of sector-wide, best-practice benchmarks and exemplars. This could be a set of model WHS policies and procedures that health services could adapt to their local conditions. In addition, WHS regulators need to improve their monitoring of remote health services’ compliance with WHS legislation and take enforcement actions to resolve the breaches.
Limitations
In the survey tool, one limitation was the lack of questions about the availability of non-clinical staff at participants’ clinics. For example, asking how many drivers are employed at the clinic would provide more information relevant to the implementation of ‘never alone’ policies.
For the safety score, providing equal weighting to all safety recommendations was a potential limitation. Recommendations considered to be a high priority by some did not generate more points when met than those seen as a lower priority. Depending on which particular recommendations were met, participants could potentially judge a workplace with a lower safety score to be safer than one with a slightly higher score. This limitation could be mediated in future studies by including an internal consistency measure. For example, the clinic safety recommendations could be followed by ‘what score would you give out of 100 for the overall safety of your clinic?’ The score nevertheless fills a significant gap in the literature by providing an objective measure of health services’ efforts to address a wide range of safety concerns.
Conclusion
This study explored the WHS strategies in place at very remote primary health clinics across several Australian jurisdictions, with a specific focus upon the experiences of the RAN workforce employed at these clinics. Notwithstanding this focus, we recognise that many of the WHS principles and practices elucidated here are relevant to other health professional groups and workplaces, particularly those working in professionally and/or geographically isolated contexts. We recommend, therefore, that further empirical research be undertaken across rural and remote Australian jurisdictions to explicate the multi-dimensional relationships between WHS legislation and concomitant policies, procedures and practices. Such research could also explore the health economic impact of both high- and low-level WHS compliance, investigate the relationships between compliance and staff recruitment and retention and, perhaps most importantly, analyse the associations between WHS compliance and the quality of care provided in these communities, as perceived by community members. Adopting a multi-professional focus would not only provide a more comprehensive understanding of the issues, but also enable greater application in areas of education, policy development and clinical practice.
In all contemporary workplaces, the presence of robust WHS frameworks and clearly articulated and transparent governance and reporting practices is now the norm for both employers and employees. By contrast, this study has drawn attention to the presence of inconsistent and fragmented policies and practices across several remote health settings, and the negative impacts upon the RAN workforce. The unique WHS challenges experienced by health workers in isolated clinical contexts require a collaborative, appropriately resourced and nuanced approach by employers, researchers, policymakers and educational organisations, to ensure that high-quality, evidence-informed practices can be readily adopted, with accountability and feedback loops in place. The workforce and the community members they serve surely deserve no less.
Acknowledgements
The authors thank Kylie McCullough, Katie R. Pennington, Sue Lenthall, Sabina Knight, Meryl Churchill, John Wright and Sue Crocker for their significant contributions to the development of this study and the survey tool. Thanks also go to Rhondda Jones from James Cook University StatsHelp, who provided statistical advice during data analysis.
Funding
The Tropical Australian Academic Health Centre Seed Funding Scheme 2020 provided $3320 funding to the Remote Area Safety Project, of which this study is a part.
The lead author received the Australian Government’s Research Training Program Fee Offset while undertaking this project.
Conflicts of interest
The authors declare no conflicts of interest for this study.

