Introduction
Diabetes is a global epidemic with 420 million cases and predicted to reach 700 million by 20451,2. Diabetes results in debilitating and chronic health complications like blindness, kidney failure, and diabetic foot complications3-6, with diabetic foot ulcers causing significant morbidity and mortality4,6-9. A diabetic foot ulcer is defined as any wound below the ankle that extends through the outer layers of the skin (epidermis and dermis) and affects subcutaneous tissue, muscle and bone, caused by neuropathy or ischaemia or both following trauma to the foot1,10,11. It is considered the most commonly and costly diabetic complication, and associated with a 5-year mortality rate of 50%11.
Diabetic foot complications are the constellation of pathological changes of the nerves and blood vessels due to the chronic insult of hyperglycaemia1,10,11. Diabetic foot complications arise from pathophysiological factors such as neuropathy, peripheral arterial disease, and impaired wound healing, manifesting in various forms including ulcers, infections, and gangrene, which can lead to significant morbidity and, in severe cases, necessitate amputation12,13. Diabetic foot complications affect 40–60 million people, with lower limbs (full or partial) lost to amputations every 30 seconds worldwide. These complications are 10–20 times more likely to occur among those with diabetes3. The global prevalence of diabetic foot complications ranges from 3% in Oceania to as high as 13% in North America, with a global average of 6.4%3,14. The global annual incidence of diabetic foot ulcers is approximately 2%, with half of those affected experiencing amputation at some stage, significantly reducing quality of life and increasing mortality1,3,11,15.
The adverse outcomes of diabetic foot ulcers and lower limb amputations affect physical, social, vocational, psychological and interpersonal aspects of their lives16. The diabetic foot results in undeniable financial burden1, equating to US$8659 (A$13,285) per person with a diabetic foot, with developed nations like America spending up to US$9–13 billion (A$13.8–19.9 billion) in total medical treatment for diabetic foot disease, which is an additional cost to diabetes treatment17.
The significance of diabetic foot complications and amputations in Fiji, despite ongoing public health action, is a concern reflected in the fact that 40% of all surgeries in Fiji are due to diabetic amputations, with one amputation occurring every 12 hours18,19. According to the Ministry of Health and Medical Service in Fiji, data from a regional hospital in 2019 showed that, out of every 12 people with diabetes with active foot ulcers attending diabetic clinics, five were referred to a treatment hospital for surgery or amputation20. This may be attributed to poor education, awareness and footcare practices among patients.
Understanding diabetic foot complications and their pathological components is important because it forms the basis of patient diabetic self-care education21. Diabetic foot complications are an underdiagnosed health problem that can easily be identified with routine foot screening and comprehensive foot care21,22. Despite extensive research on diabetic foot complications and management, there is a significant gap in understanding patients' perceptions, particularly among the type 2 diabetes mellitus (T2DM) patients in Fiji. Previous studies have largely focused on clinical outcomes and interventions, with limited attention to the subjective experiences and challenges faced by patients. To address this gap, this qualitative study aims to explore the perceptions of T2DM patients in Fiji regarding diabetic foot complications and their self-management practices.
Methods
Study design and setting
A qualitative study using in-depth one-to-one interviews of T2DM patients was conducted to explore patients’ perceptions of diabetic foot complications, as well as footcare knowledge and practices. In-depth one-to-one interviews were the preferred method for collecting data because a private interview offered a conducive, safe space for patients to express themselves without an audience. In-depth interviews are a good technique because they allow for a deep understanding of an interviewee's thoughts, experiences and perspectives. They provide rich, detailed data and can uncover insights that might not emerge in more structured methods. Additionally, they offer flexibility, enabling the interviewer to explore new topics as these arise during the conversation23.
The study was conducted from August to September 2021 at the Sigatoka Sub Divisional Hospital in Fiji, which is the referral centre for 13 peripheral health facilities in the Nadroga-Navosa medical area. Sigatoka is one of five towns in the western division and it caters to 58 931 people24. The diabetic foot clinic at the hospital, from which most of the people with diabetes were recruited, was the focus of this study.
Study sample and criteria
The study included any self-identified Fijian with T2DM aged 18 years or over. Each of the participants was required to have a minimum time since diagnosis of 6 months, and no experience of an amputation. They were individuals with either history of foot complications or asymptomatic participants. T2DM patients are chosen because they make up the majority of the diabetic cases seen in clinics, and they are more commonly affected by diabetic foot complications than T1DM patients3,14. Excluded from the study were type 1 diabetics, patients younger than 18 years, patients with cognitive impairment or known mental illness, and reluctant participants.
Diabetic foot clinics are scheduled every Friday at the hospital’s special outpatient department. However, due to COVID-19 restrictions, all routine clinics were suspended. Purposive sampling was utilised to gain insight into the perceptions of diabetic foot complications among the two interest groups: individuals with a history of foot complications and asymptomatic participants. Purposive sampling allows researchers to select participants who have specific characteristics or experiences that are relevant to the study’s objectives. Two-thirds of T2DM patients were recruited from the diabetes foot clinic patient register. Mindful consideration was given to the uniform distribution of gender and ethnic representation, hence the inclusion of T2DM patients seen in the hospital’s general outpatient department as well as those admitted at the hospital during the time of the study. Data saturation occurred when no new information was emerging from the interviews. Since all the questions were answered and no new ideas were provided by any participants, we considered 30 participants as the point of data saturation25. Five patients were interviewed per day over a 1-week period.
Data collection tool
An interview guide with pre-determined, open-ended questions as well as probing or prompting follow-up questions was used to elicit detail. The interview guide was developed based on the literature reviews and in line with the aims of this study. Reviewing other literature helped us to see how researchers worldwide have explored T2DM patients' views on foot care so we developed a new interview guide that addresses aspects that previous research focused on, aiming to cover them as well as to fill the gaps in our study. The interview guide had two sections including patient demographics and six or seven open-ended questions. The study participants were asked open-ended questions such as ‘Explain what you know about diabetes and how it affects your feet’, ‘Why is it important for diabetes patients to look after their feet?’ and ‘Have any of the doctors or nurses talked to you about foot sores in diabetes? If yes, explain what information you been given’. Probe questions were used to evoke and encourage participants to explain their answers and express their opinions openly. The interview guide, which was prepared in the three main languages (English, I-Taukei and Hindi), was tested prior to commencing interviews. The successful pilot of the interview guide was conducted among five T2DM patients; three were phone interviews and two were face-to-face interviews with general outpatients and hospital admissions. All the interviews were conducted in English because all the participants understood English and willingly expressed themselves both in English or vernacular (interpreted by their immediate family present during the interviews).
Study procedure
Considering the COVID restrictions during the time of the study, interviews were conducted over the phone for T2DM patients purposively recruited from the diabetic foot clinic while face-to-face interviews were conducted for T2DM patients purposively recruited from the general outpatient department and the hospital wards. The foot clinic patients were selected from the clinic register beginning from the most recently booked patients and working backwards. Each participant who met the inclusion and exclusion criteria and who had a valid phone number was contacted. Participants were thoroughly informed of the nature of the study, with all interviews audio-recorded. All participants who agreed to the conditions of the phone interviews gave verbal consent, which was audio-recorded. Face-to-face interviews were conducted for participants recruited from the general outpatient department and the hospital wards. All participants were interviewed at a time convenient to them, whether it was immediately when they were contacted or at a scheduled time of preference for the participant. Information sheets were provided, and written consent was obtained for all participants for face-to-face interviews, which took place in the vacant consultation room. At the beginning of each interview, the purpose and aim of the study were thoroughly explained to the participant. Participants were reassured of the voluntary nature of the study, which allowed them to exit the interviews whenever they wished. They were asked some general questions about their characteristics and health status, and these were followed by open-ended questions designed for this study. After completing interviews, participants were acknowledged for contributing to the study and further information was provided if they had any questions. Each interview lasted for approximately 25–30 minutes depending on patient knowledge or the maximum answer provided to each question. Five of the participants were more comfortable expressing themselves in vernacular so they had requested that their immediate family interpret their responses in vernacular to English.
Data management and analysis
Audio recordings were transcribed by the main researcher on the day of data collection. Recordings and transcriptions were reviewed twice by the main researcher and checked by other team members to ensure the accuracy of all transcribed information. Manual thematic analysis was conducted by reassessing transcripts to identify themes and significant data by grouping similar phrases that reflected the perceptions of the participants. Thematic analysis was conducted in the following steps: the transcripts were read and re-read to be more familiar with the data; data was then organised in a meaningful and systematic way; themes or significant or interesting data were identified; the themes were identified by grouping similar phrases that reflected the perceptions of the participants; these themes were reviewed or modified to develop subthemes. The final step involved the write-up of the research findings with the presentation of themes and subthemes supported by quotes from the transcripts25,26.
Study rigour
The study's credibility was ensured through several steps. In-depth interviews were recorded and transcribed by the researcher, with the transcripts reviewed by other team members. Peer debriefing was employed to evaluate the transcripts, methodology and findings. To prevent bias, power imbalances were considered, and subparticipants were encouraged to speak openly with the interviewer. Transferability refers to the ability to apply and compare the study’s findings in different settings. The methodology includes a detailed description of the participants and research process. Participants were chosen from a range of age, gender and ethnicities that reflect the whole population of Fiji, so the transferability of the study was achieved. Dependability was achieved through thorough documentation of the research process, allowing for replication and verification. A suitable study design was selected, and an interview guide was developed for the research. The questions were created based on a pilot study, and the interviewer, fluent in the local language, used straightforward communication methods to gather data. A systematic method was used to identify codes, subthemes and themes, with subthemes reviewed for accuracy in documenting the interviews. Confirmability was ensured by being transparent about data collection, analysis and interpretation. The interview process was reviewed by the audit trial, and the core researchers checked the data collection, transcriptions and analysis27.
Ethics approval
Ethics approval was obtained from the Fiji National University College Health Research Ethics Committee with ID#053.21 and facility approval from the Sub-Divisional Medical Officer for Nadroga-Navosa. Verbal consent was secured prior to phone interviews, and written consent was collected in person.
Results
Participant characteristics
Overall, the study included 30 participants. There were more females (63%) than males (37%); with the majority of participants aged 61–70 years (40%). There were slightly more Fijian of Indian Descent (FID) (57%) than I-Taukei (IT) (43%) participants. All participants had received formal education, the majority of whom had reached secondary school level (57%); and 84% of participants were unemployed. Many participants had lived with diabetes for more than 5 years (60%); and 50% of participants had a history of diabetic foot complication, namely callus (7%), neuropathy (20%) and previous ulcers (23%). None of the participants had active ulcers (Table 1).
Table 1: General characteristics of type 2 diabetes mellitus patients, Sigatoka Sub Divisional Hospital, Fiji, August to September 2021 (n=30)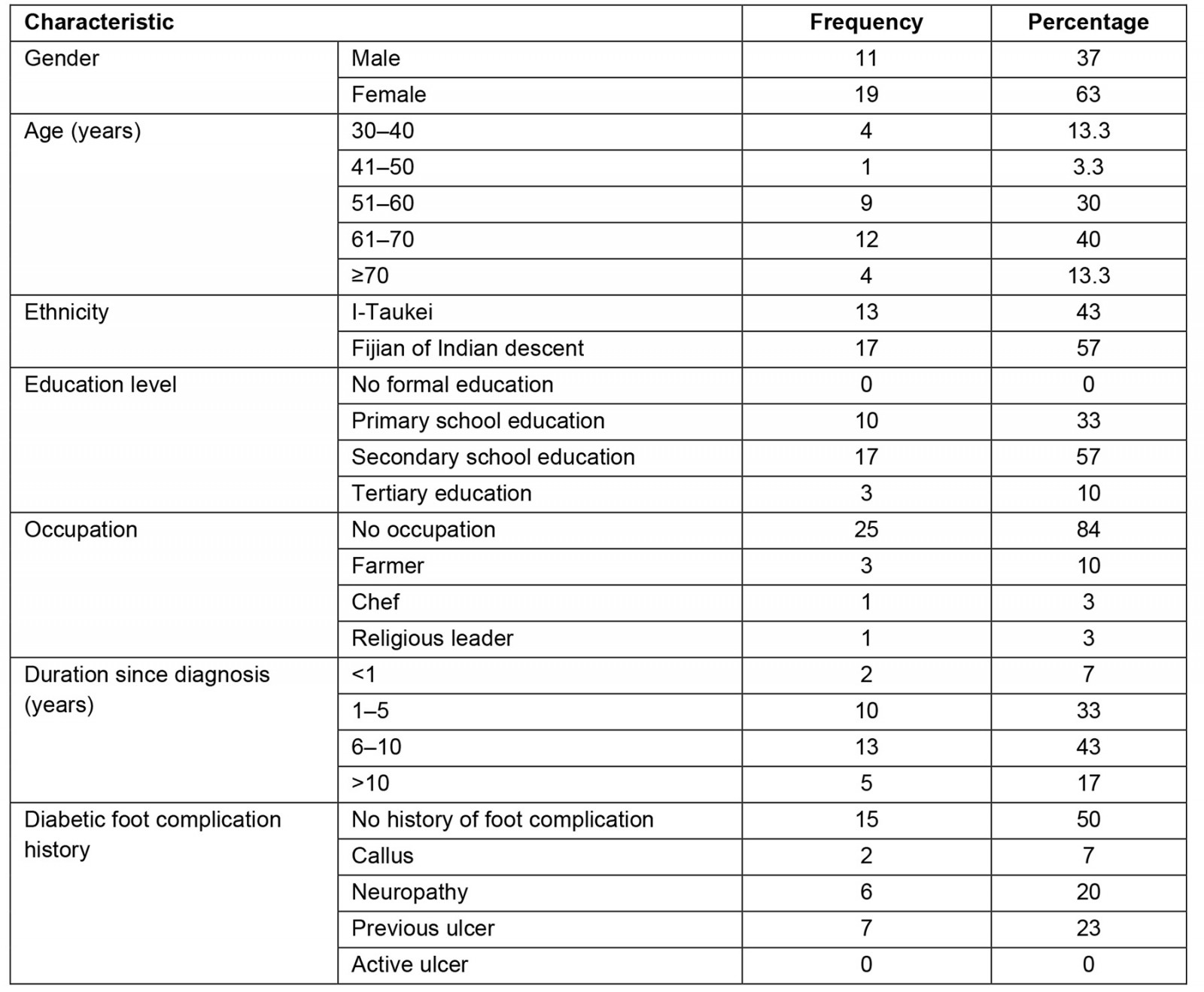
Themes identified
The thematic analysis of data resulted in three major themes: perceptions of diabetic foot complications; perceptions of footcare behaviour and perceptions of footcare services. Subthemes and categories related to each theme are summarised in Table 2.
Each of the quotations used is denoted with details of each participant (P) in brackets.
Table 2: Themes and subthemes of patient in-depth interviews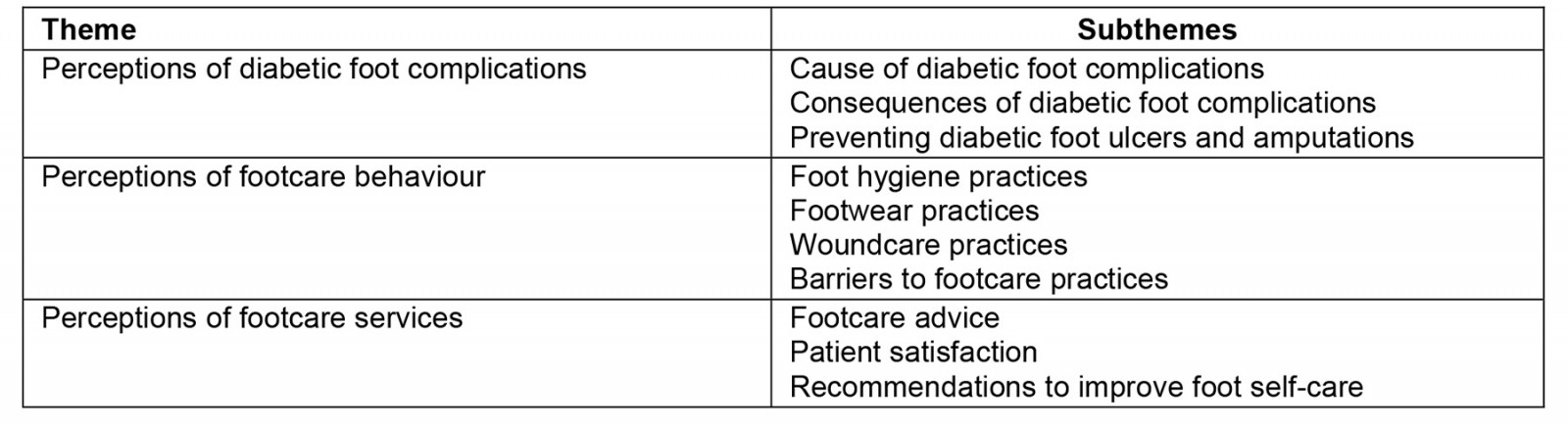
Theme 1: Perceptions of diabetic foot complications
Exploring patient perceptions of diabetic foot complications generated the following subthemes: cause of diabetic foot complications, consequences of diabetic foot complications, and preventing diabetic foot ulcers and amputations.
Cause of diabetic foot complications: There were many participant perceptions (17 patients) of the cause of diabetic foot complications. Only one participant correctly linked diabetes to neuropathy based on the advice she was given during her admission for a foot injury.
Some people they end up having numb feet and they don’t feel anything … Yeah that’s what they told me at the hospital ... but they said that if you don’t control the amount of sugar you take, you’ll end up having numb feet or you don’t do a lot of exercise just, stick around home and lie down a lot. (P5, IT female, 63)
A considerable number of the participants (12 patients) lacked knowledge on how diabetes caused foot complications. Another patients attributed their lack of knowledge to the absence of symptoms and their low perceived risk of diabetic foot complications.
I don’t know how, because it doesn’t affect me. (P6, IT female, 36)
The majority of participants (20 patients) perceived foot complications in terms of their symptoms and its relation to their blood sugar levels.
When my sugar is … like more than 17 or 18, then I feel my feet paining, and like paining like chilli. (P22, FID female, 58)
A small number of participants (seven patients) attributed diabetic foot complications to risk factors, such as unhealthy diet and lack of exercise.
They should cut down the sugar, they shouldn’t eat too much root crops especially the cassava. They should rely on breadfruit, the banana, the vudi [wild banana] and the rice. And to do plenty exercise to burn down the sugar. (P11, IT male, 63)
The ‘cold’ was also perceived as a contributing factor to diabetic foot complications.
I’ve got pain in my legs, in my nails … I don’t have any injuries in my legs but it’s painful and itchy. I don’t know what it happens. Maybe it’s because of the cold together with the diabetes. (P21, FID female, 51)
Participants’ perceptions of diabetic foot ulcers did not vary between individuals with a history of foot complications in comparison to asymptomatic participants. Overall, a third of participants had no notion of diabetic foot ulcers. Commonly identified factors between the two groups of participants (individuals with history of foot complications versus asymptomatic participants) include poor hygiene.
When it is dirty, it turns into sores and starts rotting and all these things. Even the nails when they’re too big and the overgrowth underneath the nail harms the skin. And if you walk barefoot you’ll get hurt and that will turn into major problem. (P20, FID female, 61 – no history of foot complications)
Patients perceived careless behaviour resulting in injury that causes diabetic foot ulcers.
We just walk barefoot, no shoes on the legs and don’t bother about that. Maybe the pin [something sharp] punctured the area, and the sore started from there. That’s the main thing. We are affected from the leg, the diabetes start. The cutting of the legs just from our carelessness. (P21, FID female with peripheral neuropathy, 51)
Participants perceived a low risk of diabetic foot ulcer despite the presence of peripheral neuropathy.
It’s numb [her feet]. I’ve got the hard skin on my foot. Last Friday I cleaned that one … I haven’t got the sores so I don’t know. (P26, FID female, 60, with peripheral neuropathy)
Participants attributed lower limb amputations to unhealthy diet, late presentation to the hospital and carelessness.
Because when we don’t care about the food. And if it starts you have to go to see the doctor. If you take time, stay home few days then the poison starts and it starts rotting. (P21, FID female, 51)
Consequences of diabetic foot complications: Low perceived risk for foot complications affects patient perception on the need for routine foot checks.
Nothing is wrong with my feet. I always go there [to hospital] and take my tablet because nothing happens to my feet, I don’t check regularly with my feet. (P6, IT female, 63)
However, the same participant was fearful of getting an amputation, which explains her precautions.
And I’m really taking precautions [laughs] not to get my foot amputated or something. It’s just like that. I think the diabetes can be reversible. (P5, IT female, 63)
Personal or family experience of diabetic foot complications can contribute to participant knowledge of the consequences of diabetic foot complications.
My neighbour, one lady, she had you know sweet blood. And she had a cut on the bottom of the foot. And that gradually, you know, it gone up, up, up. So you know cut the leg here, cut the leg here, cut the leg here [gestures to different levels of his leg]. So they do not take care of it in when the first day they got the nail or whatever it is [injury to foot]. And because that lady, they go barefeet in the poultry and here and there … they get the injury. (P15, FID male, 75)
Participants perceived disability as a result of lower limb amputations that can seriously affect their lives.
Well our feet is very important to us. Because if no feet we can’t do anything. So we have to look after our feet. (P22, FID female, 58)
Preventing diabetic foot ulcers and amputations: Participants’ perceptions on preventative measures for diabetic foot ulcers and amputations include adherence to personal hygiene, diet control, and footcare practices.
Well I know we have to look after ourselves and look after the food, look after what is going inside our mouth. And we have to be clean all the time, don’t let the perspiration stay in your body. And wash it nicely so it doesn’t turn into sores. Wear shoes all the time, clean your feet, wash your feet, watch your feet when you are bathing. And never get out of the house without shoes on. That’s it, be clean. (P20, FID female, 61)
Participants discussed that diabetic foot ulcers and amputations can be prevented by timely presentation to health facilities for medical treatment.
If I got a cut from my feet I should go to the hospital as soon as I get it, not having a cut and staying home until it’s worse and then go to the hospital. (P3, IT female, 57)
Dietary habits and practice were well explained by most of the participants.
Take small amount of food, don’t take too much. But you can have a little but portion like 3 times to 4 times a day. Don’t take too much, small amount only. When you want to eat, eat little bit like bean or something like that. Just to fill the gap. (P11, IT male, 63)
They perceived that compliance to medications can help prevent amputations.
If I don’t look after my diet. If I don’t have tablets at the right time I can lose my toe. (P7, IT female, 65)
Theme 2: Footcare behaviour
Some questions generated subthemes on patient footcare behaviour such as foot hygiene practices, footwear practices, woundcare practices and barriers to footcare practices.
Foot hygiene practices: Participants had different self-care practices such as wearing suitable shoes and washing feet to protect their feet.
I always wear my shoes. Whatever work I’m doing, gardening. So I try to be careful with my feet. So, after the day when I have my bath I try to wash my feet nicely every day. (P11, IT male, 63)
Another participant had help and guidance from family, who ensured foot self-care practices were followed.
My daughter is a like a doctor. She takes care of me a lot. I wear shoes at all times. Limited activities. She would not allow me to leave the house and go around the garden, or just roam about around the house. And no sugar, no sweet drinks. (P15, FID male, 75)
Some participants relied on healthcare workers (HCWs) to assist with foot care.
I used to come around and see the footcare nurse … because she knows it very well [patient attends foot clinic to cut his toenails and clean calluses]. So once I saw the skin is getting thicker, so I go and see them. (P2, IT male, 70)
Participants stated that using sharp tools like scissors or a razor blade to cut toenails is not advised, because there’s a high risk of causing injury to the foot.
I cut toenails with scissors and trim it with sand paper. (P15, FID male, 75)
Footwear practices: Some participants stated that they wear shoes at all times to avoid injuries.
Checking the feet every day. I just wear the shoes every time. I go in the farm, I wear the shoes. I cross the river or go in the town, I wear the shoes. (P8, IT female, 60)
One of the participants was aware of the importance of wearing footwear, but did not practice it indoors.
Yes, I should wear flip flop everywhere I go to make sure the nails like that doesn’t poke it. No, I don’t wear it in the house. (P12, IT female, 36)
Misconceptions of safe footcare practice were conveyed by the son of a participant.
Yes, she has her own socks and gumboot. And sometimes she just puts on the plastic just to protect her foot and then she puts on the boot … this was her own initiative. (P10, IT female, 51 – interview interpreted by son)
Wound care practices: A participant shared his experience with wound care at home by presenting immediately to the hospital for treatment.
I was at home when I got the nail in the flip flop. I came straight to hospital and got injections and medicine. (P15, FID male, 75)
Despite the availability of conventional medicine, patients still opt for traditional medicine as their first line of treatment.
She only stays home and uses Fijian traditional medicine … Traditional medicine used for both sugar control and healing of sores on her feet. (P10, IT female, 51 – interview interpreted by son)
A participant explained that choice of treatment and current lifestyle now is due to religious influence that has benefited her.
When I was just discharged from the hospital, I had some of those friends who were Seventh-day Adventist Church. They came to advise me on my diet and what I’m supposed to do. So they helped me with these charcoal drink. So we prepare the charcoal drink and they showed me what’s the recipe … I’m trying to control my diabetes. (P5, IT female, 63)
Barriers to footcare practices: Some of the patients were reluctant to present to hospital due to COVID-19.
You know because of this pandemic, he doesn’t want come around to hospital anymore because COVID. (P14, FID male, 38)
Some of them had low perceived need to practise foot care due to the absence of diabetic foot ulcers.
Because my sores has healed a long time ago, so I don’t, I just wear shoes whenever I’m moving around. (P5, IT female, 63)
The suspension of routine the special outpatient department and foot clinics was one of the barriers to footcare practice.
There’s a wound under my foot for 2 to 3 years now. It’s a very small one now, but normally the skin goes thick [callus] … I used to come around there they used to give me the date to come around. But now the COVID eh, I’m not going around there [hospital] anymore … Well at the moment I don’t have any special dates to come around and check my foot. (P2, IT male, 70)
One of the issues raised by the participants was stigma. A patient had significant weight loss due to his diabetes, and was ashamed of attending the special outpatient department and foot clinics because of this.
He was a big man before, now he’s losing weight his weight is same of his daughter staying at home. So it’s like he’s ashamed to face some of the people lining up because plenty people knows him because he’s a farmer. So when he’s losing weight like this he becomes ashamed of himself. So himself he’s not taking the medicine, he’s taking the injection. So I’m asking him you have to go and bring the injection for yourself. And he’s ashamed of himself lining up there to take numbers to go and take his medicine. (P9, IT male, 36 – interview interpreted by wife)
Theme 3: Patient perceptions of footcare services
Since health education and awareness rely mainly on communication with patients and HCWs, this theme explored patient experience of footcare advice received, patient satisfaction with healthcare services received and patient recommendations to improve foot self-care.
Footcare advice: Most of the respondents received footcare advice from HCWs during special outpatient department visits. Participants who denied receiving any form of footcare advice obtained footcare knowledge from alternative sources. One participant obtained information from reading material he received from the hospital.
No [denies receiving footcare advice]. I just read a book from the hospital. (P11, IT male, 63)
Another participant was advised by her mother on footcare practices:
[received footcare advice from] My mother, because my father has got the diabetes … Clean, dry every time. (P26, FID female, 60)
Some received advice on diet, exercise and footwear.
Yeah they said if I don’t control my diet I can get worse than that, it can affect my body. So they told me what I’m supposed to take and what I’m not supposed to take. And the amount of food each meal. And exercise … But whenever you go out you have to wear your shoes because some people they end up having numb feet and they don’t feel anything. (P5, IT female, 63)
Participants were advised on the need to present early to hospital with any injuries, and the expected outcome if foot infections are worse.
She told me if you get one cut in your foot as soon as you get the cut you come straight to the hospital. So that they can, the doctor and nurses can fix it and give the injection or tablets before it gets worse. If it gets worse you can get your leg amputated. (P3, IT female, 57)
Patient satisfaction: Most participants were generally pleased with HCWs’ approach and services to patients.
Yeah, I’m happy [with the HCWs]. Something we don’t understand they explain. (P13, IT male, 74)
However, one participant voiced his dissatisfaction with HCWs’ attitudes.
Clinics are ok, but some of the staff they talk rude. (P14, FID male, 38)
Participants were happy with the holistic care service provided by HCWs.
They check the blood, sugar level, eyes, and tablets are provided. (P16, FID female, 58)
Another participant expressed approval of the frequent foot checks that were conducted with every visit.
Nearly every time I visit. The doctors see, the doctors gets up and tells me to take off the shoes and he watches. Yes, confirms checking for sensation. With a pen and even with their bare hands … I’m very happy with the clinic. (P20, FID female, 61)
Recommendations to promote foot self-care: The study participants highlighted the importance and role of HCWs, suggesting that they should adopt a holistic approach when visiting T2DM patients in the special outpatient department. They believed that a comprehensive and holistic approach is essential for effectively helping patients in the hospital.
If we have a like a boil or something like that the doctor told us to go to the outpatient. Just my point of view, that doctor should treat everything. That doesn’t suit because we sit 3 to 4 hours for our clinic. (P18, FID female, 58)
Some participants thought there should be more healthcare advice during special outpatient department clinics.
They have to check regular check-up with our sugar. They have to tell us the right amount of food we take and what amount of thing we have to take. (P6, IT female, 63)
Introducing tele-consultation would be helpful for patients during the COVID-19 health restrictions that temporarily suspended routine special outpatient department clinics.
I think because of this pandemic … he doesn’t want to visit hospital most of the time because of the situation. I think it’s good if we have certain doctors who can call us, advise us, and make a record of everything. (P14, FID male, 38 – wife sharing their experience)
Some participants stated that having more outreach programs for community awareness is helpful.
They have to come to the village … and give the information to the people. (P13, IT male, 74)
Overcrowding of special outpatient department clinics was highlighted as an area of weakness, so a participant suggested having clinics over 2 to 3 days and redistributing patients evenly to provide optimal care.
The clinics are overcrowded. Oh yes, like we wait from the morning until the evening. If they can give us 2 days or 3 days [smaller groups of patients] so we can be thoroughly checked. (P11, IT male, 63)
Two other participants voiced similar complaints on the long waiting time for special outpatient department clinics.
So when they go, they have to wait in a long line. (P16, FID female, 58, and P17 FID male, 52 – interview interpreted by their daughter)
Some were concerned about enough medications being dispensed to patients.
To give us more tablets [adequate supply]. (P7, IT female, 65)
Others mentioned the importance of ensuring accurate clinic dates are given to patients to avoid miscommunication.
I remember that 2 times it happened in the small booklet for clinics, sometimes maybe we are too crowded to be checked. And they gave me the wrong date. They write it on the book. Just what they wrote in the book was wrong. The date to get the next clinic. (P11, IT male, 63)
Some of them suggested involving family members in their treatment plans to ensure continuity of care at home by the family.
I think the only thing you can do is whenever a patient is admitted you get the family to talk to them regarding the looking after of that patient. Yeah some are minor ones and some are very severe. Now those ones they need people to look after them. So their families should be involved. To explain to them what they are supposed to do, what food they have to give and what food they’re not supposed to give. (P5, IT female, 63)
Discussion
This study aimed to explore the perceptions of T2DM patients in Sigatoka, Fiji, on diabetic foot complications and their management. The results of this study, concentrated on three main themes – patients’ perceptions of diabetic foot complications, footcare behaviour and footcare services –will be discussed here.
Patients’ perceptions of diabetic foot complications
Overall, there was lack of knowledge about diabetic foot complications despite participants’ awareness of other aspects of diabetes care, especially knowledge on dietary advice. They explored their own experience of foot complications, including symptoms and contributing factors like unhealthy diet, lack of experience and misconceptions such as the concept of 'cold’. They described careless behaviour that led to injuries and peripheral neuropathy, contributing to foot complications. Additionally, they linked lower limb amputation to factors such as poor diet, delayed hospital visits and carelessness, reflecting a range of negative experiences related to foot complications. Diabetic foot complications were poorly understood by most of the participants in other studies16,28. Findings such as the role of personal and family experience on patients’ knowledge of diabetic foot complications, and ignorance among participants without foot abnormalities, were underpinned by Bossman et al28.
Participants had low perceived risk of foot complications, with associated low perceived need to attend foot clinics; they expressed fear of amputation; and had lack of personal experience with lower limb amputation, and with disability as a result of amputation. All of these are corroborated in previous literature16,28,29. Some preventative strategies outlined by participants include adherence to footcare practices, timely presentation to health facilities for medical treatment, diet control and compliance with medications. These demonstrate both their correct knowledge and their understanding of the importance of preventive measures to enhance their health status.
The results of this study highlight the need for improved footcare awareness and education among patients. Provision of pamphlets with footcare information, as well as utilising pictorial and teach-back teaching methods during special outpatient department clinics for patients as a form of educational strategy, which has proven to be effective in patient education.
Patients’ perceptions of footcare behaviour
Barriers to footcare identified by respondents were mainly related to the impact of COVID-19 on routine special outpatient department and foot clinic services, which were suspended during lockdown30. Respondents were avoiding hospital presentations for diabetic foot infections and other foot-related issues, fearing that they could contract COVID-19 by doing so. The low perceived need for footcare practice was expressed by 10% of the respondents, which is similar with other studies31,32. A misconception of safe foot self-care hygiene practices was expressed by the participants. Other respondents had reasonable footcare knowledge, but described some hazardous self-care practices they were engaged in that they ‘thought to be’ safe31,33. There were knowledgeable respondents who were aware of proper footcare practices, but did not adhere to them due to the low perceived need to look after their feet30. These factors can be identified as contributing factors to delayed health-seeking behaviour, with late hospital presentations resulting in severe diabetic foot ulcers that lead to amputations34. It is essential to organising multidisciplinary (doctor, foot clinic nurse, dietician, physiotherapist) outreach programs for all medical areas within the Nadroga-Navosa subdivision to screen remote communities and provide footcare education and awareness. The findings also highlight the need for better planning by the Fiji Ministry of Health and Medical Service during epidemics and pandemics so that other crucial services in healthcare delivery are not affected, such as the special outpatient departments, as seen during the COVID-19 pandemic.
Patients’ perceptions of footcare services
Footcare advice received from HCWs was fairly well perceived by the respondents. The majority of respondents received footcare advice from HCWs during special outpatient department visits. Also, they expressed basic knowledge about foot care in relation to foot hygiene, like washing their feet and wearing shoes. This may have been commonly mentioned due to its association with daily activities like bathing, which is associated with washing of the feet; and farming or gardening, which are associated with wearing footwear outdoors. Very few respondents talked about nail care and footwear. All respondents lacked adequate footcare knowledge on self-examination, which is key to patient identification of danger signs, and this lack of knowledge may delay health-seeking behaviour31,32,35. Only one respondent had generally adequate knowledge on diabetic foot complications and foot care compared to others, which she gained during her hospital admission for her foot complication. This supports the study of Matricciani and Jones, which showed that the provision of footcare education was associated with a reduced risk of foot complications in high-risk individuals31.
Many studies with T2DM patients and their footcare behaviour have shown that education significantly enhances patients' foot self-care behaviours, self-efficacy scores and perceived footcare behaviour, while also reducing the prevalence of foot risk factors. Additionally, these studies demonstrate that education improves patients' knowledge, willingness, and motivation to learn and change behaviour36-38. For respondents who denied receiving any form of footcare advice from HCWs, their source of footcare information was from reading materials from hospital, their family members and family experience. The latter is evidence of the importance of family involvement in patient care and support31,39. Regular in-house teaching sessions among HCWs by trained footcare nurses on diabetic foot complications and foot care is needed.
The results of the present study indicate that most patients believed HCWs should offer a comprehensive and holistic approach, including necessary services and advice during visits to the special outpatient department clinic. Additionally, patients felt that having clear and accurate clinic dates was essential to prevent miscommunication. These recommendations from study participants aim to enhance communication between patients and HCWs, ultimately improving patients' knowledge and adherence to diabetes management and care practices. Healthcare system barriers such as long waiting times and high diabetes treatment costs outlined by Suglo and Evans33 elicited mixed feelings for HCWs, which is reflected in the present study. Respondents identified HCWs and the clinics as an integral part of their care through the services provided, the education received and the medications provided. Holistic care is replaced by rushed consultations due to time constraints, and overbooked clinics with long queues and prolonged waiting times demotivate patient attendance and treatment adherence33,40.
Despite the availability of conventional medicines in the hospital, the study participants preferred traditional medicine as their first line of treatment due to their cultural backgrounds and traditional perceptions. This preference presented a challenge that impacted patients' diabetic foot care. The result of this study is in contrast with the other studies. Non-availability of medications was considered as a demotivating factor for patients who had to purchase their own medications33. Improving service delivery by ensuring that there is adequate medication for the patients should be considered. Adherence to medication improves glycaemic control, which is an essential aspect of diabetes management and foot care, while uncontrolled blood glucose levels gradually lead to diabetic peripheral neuropathy, among other diabetes complications41. Opportunistic footcare screening through mobile foot clinics and early detection may reduce foot complications.
These system barriers can be addressed by implementing staff training to decentralise foot care to peripheral centres, redefining HCWs’ roles to include footcare practice in their job description, to avoid HCWs shifting responsibility to trained footcare personnel42. Teleconsultations have emerged from the COVID pandemic as traditional face-to-face consultations were interrupted by lockdown and movement restrictions30. Also, family involvement in patient care is one of the ways of improving adherence to foot care and T2DM management31,39. Conducting research on a larger scale to gain more insight into diabetic foot care and practices in Fiji is essential. This study also shows the importance of a follow-up study on the effectiveness of patient education, family member involvement, and HCW support and teleconsultation on patient foot care.
Limitations
This study has a few limitations. First, it was conducted in just one hospital in Sigatoka, so it would be useful to replicate this in other hospitals across Fiji for broader results. Second, the study focused only on patients, but including HCWs could provide insights into their roles in supporting patients' dietary care. It would also be beneficial to involve decision-makers like the Fiji Ministry of Health and Medical Service. Additionally, while the role of family was noted, we didn’t interview family members. Including their perspectives could offer a deeper understanding of the food care challenges patients face. Due to COVID health restrictions, face-to-face interviews had to be substituted with phone interviews for most of the participants. The limited cellular reception in some of the rural areas inland may have also influenced the residential distribution of participants to include those residing in urban and coastal areas.
Conclusion
Diabetic foot complications and resultant amputations are a growing source of morbidity and mortality resulting in the reduced quality of life of affected individuals. This study revealed that diabetic foot care was a low-priority aspect of diabetes self-management, compared to glycaemic control and diet control, which were commonly reiterated through the advice delivered by HCWs, family members and the community. Preventative measures for diabetic foot ulcers and diabetes-related amputations were poorly perceived; and patients attributed them to carelessness, poor hygiene, the ‘cold’ and mainly an unhealthy diet.
Based on the study’s findings, several recommendations can enhance foot care among T2DM patients in Fiji. Patients should actively seek opportunities to improve their knowledge, adhere to their medications, and consistently follow the advice of their doctors and healthcare centres. HCWs should offer a comprehensive approach, including regular follow-ups on treatment and practices. They should focus on educating patients about foot complications, prevention and care. Additionally, improving clinic booking systems, ensuring accurate consultations and incorporating digital health tools like teleconsultation for follow-ups are crucial. Involving family members in patient education in Fiji is also recommended.
Acknowledgements
We appreciate the time and support of all the study participants.
Funding
No funding was received for this research.
Conflicts of interest
The authors declare no conflicts of interest.



