Introduction
In an ever-changing world, the most significant challenges for effective primary health care (PHC) lie in focusing on the interpersonal aspects of care, the concerns and expectations of patients, their sense of dignity, and their participation in decision-making. Furthermore, the severe economic crisis and recent global conditions, such as the global pandemic, have highlighted the importance of the role of PHC, especially in low- and middle-income countries and Greece1.
In this context, the transformation of PHC services is recognized as a top priority, with the involvement of patients in improving health care being a key necessity, as pointed out by WHO2. The involvement of patients in the evaluation of healthcare services necessitates the availability of scientifically sound instruments that facilitate valid and relevant data collection3. Recent literature has witnessed a rapid growth in research interest, and the widespread availability and use of quality indicators and instruments designed to measure patient experiences or satisfaction with GPs, ultimately aiming to inform patients, providers, and policymakers about the quality of health care4,5. Furthermore, a value-based health care designed to focus on quality of care and provider performance is of special medical international interest and importance, with patient experience being one of its fundamental pillars.
The ‘value’ in value-based care refers to what an individual values most. Patient experience, as a core component of value-based care, reflects the quality of care delivery and directly impacts health outcomes and patient satisfaction. By integrating patient perceptions into PHC, healthcare systems can better understand patient needs, preferences, and satisfaction levels, thereby enhancing the quality and effectiveness of care delivery. This international perspective underscores the universal relevance of prioritizing patient perceptions in PHC policy and practice, aligning with the overarching goal of improving healthcare quality and outcomes worldwide.
In Greece, PHC was initially developed in rural settings with the establishment of health centers. Restructuring PHC services, evaluating patient needs and views, and ensuring quality have been recognized as high priorities by previous Greek governments. A new primary care Act has been passed by the Greek Parliament and, since October 2022, has brought several changes regarding a holistic approach to citizens' health and the system of electronic personal doctor appointments, which have been activated. In Law 4931/2022, the ‘personal doctor’ is established, providing comprehensive and continuous care for every citizen, with a focus on prevention and health promotion. Personal doctor services include:
- managing the most common chronic conditions, major risk factors, and health care and rehabilitation services. Moreover, it involves coordinating with other specialists in the local health network as appropriate and with referral hospitals
- providing patient support and responsible guidance within the health system
- implementing prevention and screening programs, as well as monitoring vaccination programs
- referring patients to other specialists, and diagnostic tests, including preventive services and screenings, as defined by specific guidelines and protocols determined by the Ministry of Health based on international standards
- continually monitoring their patients, recording and updating their medical history in the digital health record, ensuring continuity and coordination of health care.
In this new organizational and political context in Greece, it is worth further addressing the relationship between patient experience and satisfaction to promote healthcare system resilience in light of potential healthcare crises, helping to identify those aspects of healthcare experiences that matter most to patients2,6,7. Moreover, it is of high interest to explore patient preferences for PHC services and their GPs, as well as to assess patient views on PHC provision. Furthermore, it is essential to explore aspects of PHC delivery valued by patients after the economic crisis period and the significant PHC reforms in Greece. Thus, insight into patient priorities for the healthcare system may support decision-making on desirable models for care provision in general practice. In this sense, patients are the ultimate judges of whether the care provided has helped them improve their health and quality of life. In this view, not only the outcomes of care, such as health benefits or met needs, are significant, but also how care is provided: the doctor–patient relationship (attitude of care providers and their communication with the patient), medical care, information and support, organization of services, and accessibility of care.
Data relevant to the evaluation of PHC services in Greece are scarce. A qualitative study based on semi-structured interviews has been implemented in rural Greece, involving 21 PHC centers in two regions of Greece8. The main identified barriers to providing high-quality PHC services were PHC service shortages in workforce and equipment, inadequate GP and paramedic training, the absence of position/job descriptions or duty statements for GPs and other PHC personnel, and limited public awareness about the role of GPs. In 2017, a Greek cross-sectional study9, not only validated the European Task Force on Patient Evaluations of General Practice (EUROPEP) questionnaire, but also explored how economic crisis conditions have affected patient priorities, views, beliefs, and trust in public PHC services, and further examined the extent to which PHC succeeds in meeting the needs of patients. Primary healthcare reforms, like many reforms internationally, are being implemented by the Greek government. For fair priority-setting, decision-makers should consider relevant evidence and reasons, so patient experience evidence should not be ignored. Since patient experience is required for a decision-making process that considers all relevant evidence, it is crucial to support available information from the past by addressing here the following research question: ‘Is there patient experience evidence to support the decision-making processes taking place in the context of the primary care reform in Greece?’
This article reports EUROPEP data from 16 PHC centers in rural settings before the most recent PHC reform in order to provide baseline information and input for future policymaking comparisons in Greece. Additionally, this study anticipates exploring to what extent EUROPEP could be a tested metric instrument for the indirect assessment of the personal doctor reform in both rural and urban settings.
Methods
Design
The Greek version of the EUROPEP instrument and data from a Greek cross-sectional survey in general practice9 were used to give insight into differences in patient views of the healthcare system in the post-crisis period and explore current patient needs. Vova-Chatzi et al assessed the psychometric properties of the Greek version of the EUROPEP, pre- and post-crisis, and estimated GP-level reliability for scales9. The Greek EUROPEP remains relevant after the economic crisis, notwithstanding new financial statements and a reliable, useful key measure to policymakers10. Based on a representative sampling frame described by Vova-Chatzi et al9, 532 patients participated in the study.
Data collection and study context
The research was conducted across the 16 PHC centers of Epirus, which is one of the seven healthcare regions in Greece, from June to September 2017. The region of Epirus lies on the north-western corner of the Greek mainland and is a mountainous, sparsely populated, poor and isolated rural area ranking among the top 20% of the OECD regions for health10. The collected data first underwent screening for factorability9. In the present article, this dataset serves as a baseline, offering valuable information and insights to facilitate future policymaking comparisons in Greece.
The reference population for sample selection comprised people who visited the PHC centers weekly during working days. The questionnaires were distributed during the waiting time before or after the examination, were anonymous, and the participants filled out the questionnaires. Comparisons between patients with and without chronic disease were also made since it is assumed that experiences and satisfaction are expected to differ across these patient subgroups for PHC services in Greece.
Instrument
To serve the purposes of the study, data collected with the EUROPEP tool was used, since this instrument is considered one of the most suitable European tools for surveying patient opinions in relation to the GP and the PHC centers11,12. The Greek version of EUROPEP, like the original one, uses a five-point Likert scale (1=‘bad’, 5=‘excellent’, which correspond to ‘very dissatisfied’ and ‘very satisfied’, respectively). The questionnaire includes 23 items concerning five aspects of health care that ask patients to evaluate their regular GP, taking into consideration their experiences over the last year12. The questionnaire also includes five background questions regarding age, gender, self-rated health, number of consultations over the previous 12 months, and the existence of chronic disease (lasting more than 3 months)12.
Vova-Chatzi et al identified three domains (clinical behavior, support and services, and organization of care) in the Greek EUROPEP that had acceptable construct validity evidence and internal consistency reliability9. In addition, the very satisfactory derived psychometric properties ensured high data quality and that the scales seemed to capture the full range of potential responses in the population. Thus, differences in patient views and changes over time in different economic contexts can be detected effectively since the EUROPEP was found to be robust9. For more details regarding the Greek version of the EUROPEP, the properties and the evaluation of this instrument, see Vova-Chatzi et al9. Within this frame of reference, we used the EUROPEP to assess patient expectations, views and perceptions of a rural and remote population that experienced the economic crisis intensely.
Statistical analysis
Characteristics of participants were summarized using descriptive statistics. Univariate comparisons were performed for patients with and without chronic disease, using Pearson’s χ2 for categorical data. All analyses were conducted using the Statistical Package for Social Sciences (SPSS) v22 (IBM; https://www.ibm.com/spss).
Ethics approval
Ethics approval was provided by the Ethics Committee of the University Hospital of Crete, and clearance to run the study was offered by the Greek Ministry of Health (protocol number 9919). The dataset only contained anonymous data. Patient participation was voluntary and anonymous8. Informed consent was obtained from all subjects involved in the study.
Results
Demographic characteristics
Table 1 presents the sociodemographic characteristics of the patients sampled. Almost half of the respondents were male, and the other half were female. Nearly 82% (437) of participants were aged ≥66 years. Close to half (276 participants) reported that they had graduated from high school (≥12 years of formal education) and were in good or very good health. Almost 78% (416) of respondents reported up to six GP attendances last year, and almost 93% (494) of respondents reported the presence of chronic disease.
Table 1: Sociodemographic characteristics of respondents to European Task Force on Patient Evaluations of General Practice questionnaire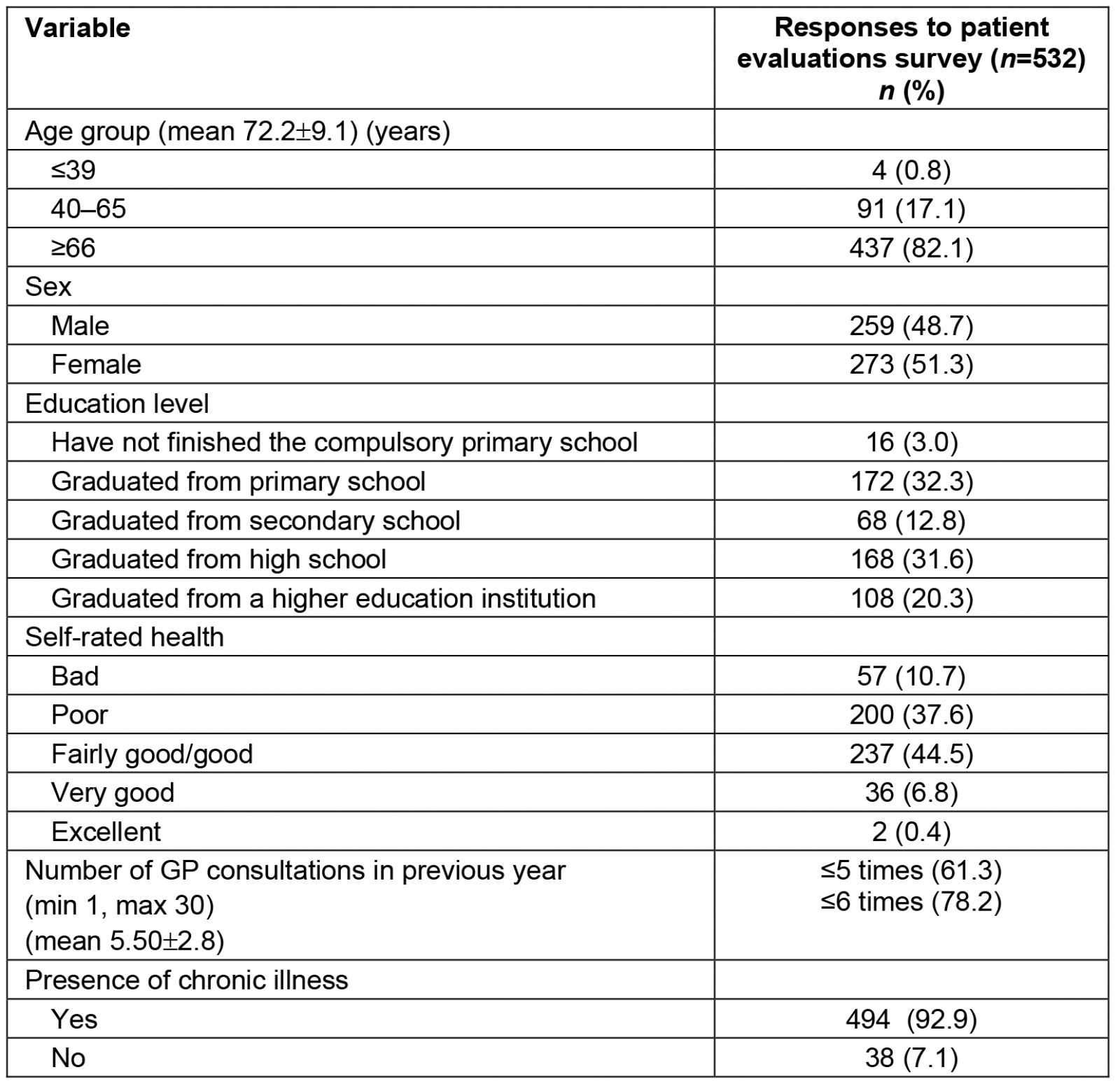
Health status and primary care service use patterns
Table 2 presents information on the health status of patients and PHC service use patterns for the overall sample and those with and without a chronic illness. Almost 52% of participants described their health status as fairly good / good or very good / excellent. Self-rated health status for individuals with a chronic disease was reported as worse than that for individuals who did not have a diagnosed chronic disease. During the study period, three out of five participants had consulted a GP more than five times in the previous 12 months. Among patients with chronic illness, the proportion of patients with five or more consults increased to 64% (p<0.0001). Among patients sampled, only about 3% of patients with a chronic disease strongly recommended a GP or reported they would not change GP compared to 23.7% and 18.4%, respectively, of patients without a chronic disease.
Table 2: Participant health status, frequency of GP visit, and intention to change or recommend GP overall (n=532) and by presence of a chronic disease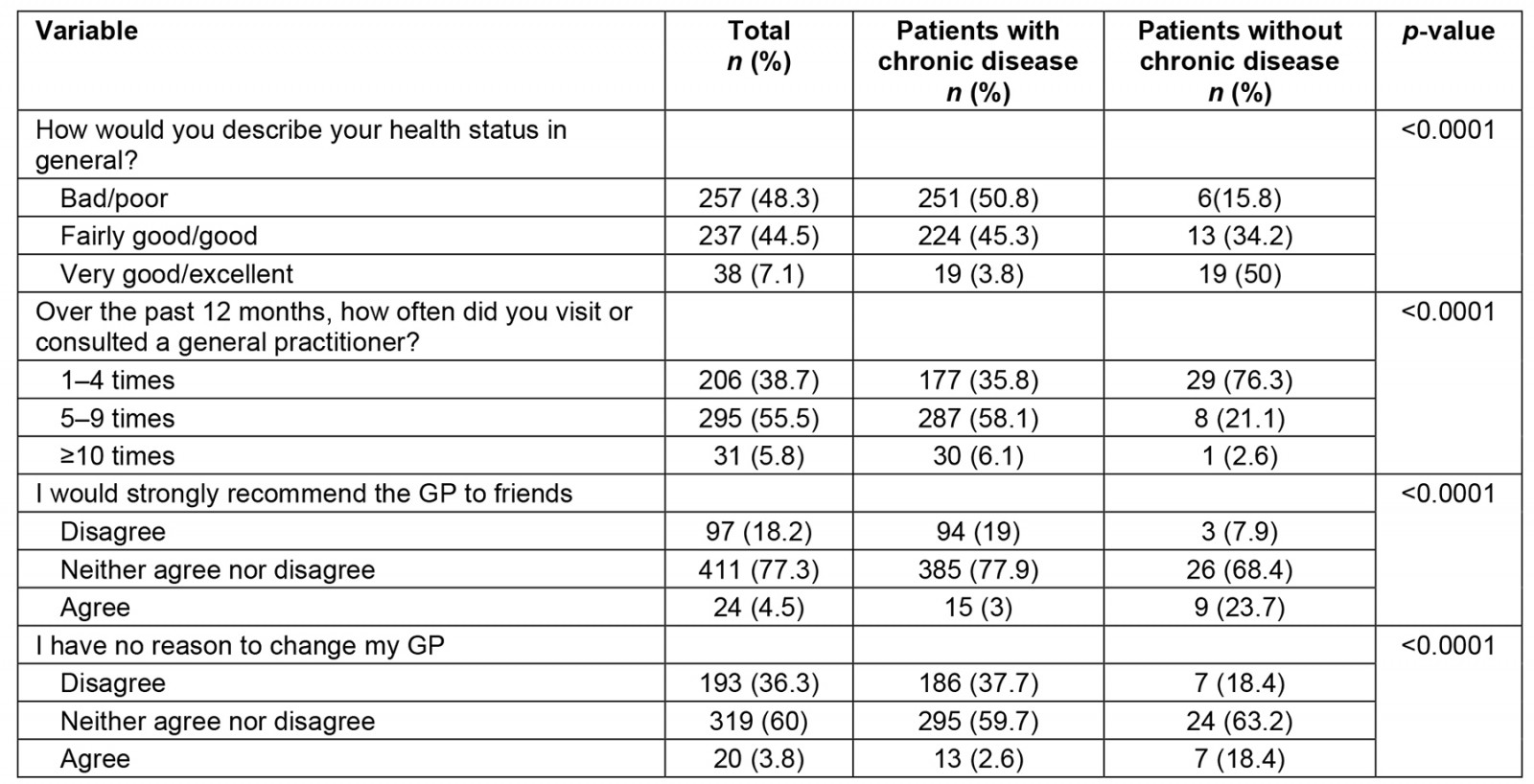
Patient experience questionnaire
Tables 3–5 present the results regarding participant experiences at the GP consultation at which they were surveyed for each of the three main domains (clinical behavior, support and services, and organization of care) assessed. Patients were asked to evaluate their GP on a five-point scale (1–5) ranging from 1 (‘bad’) to 5 (‘excellent’) (2, 3 and 4 had no text). All items were scored in the same direction, and higher scores represented better experiences (1 and 5 correspond to ‘very dissatisfied’ and ‘very satisfied’, respectively).
Patient responses were recoded for simplicity: ‘1 (recoded)’ combines 1 and 2 scores of Likert items; ‘2 (recoded)’ corresponds to response 3 on the Likert scale, and ‘3 (recoded)’ combines Likert scores of 4 and 5. Acceptable floor and ceiling effects were observed (the ceiling and floor effects were all less than 15%, and ranged from 0.6% to 3.2% and from 0% to 8.6%, respectively) allowing this encoding of categories. The main findings are reviewed for each domain below, focusing on the percentages of positive patient evaluations of general practice care, ‘3 (recoded)’.
Clinical behavior
Small percentages of participants felt that the GP spent enough time with them during consultations (4.3%); the GP was interested in their personal situation (3.9%); was helpful with their personal problems (4.3%), concerns and emotional problems related to their health status (4.3%); included them in decisions about medical care (3.4%); explained the purpose of tests and treatments (5.3%); helped them understand their symptoms and/or illness (4.9%) as well as the importance of following his/her advice (4.5%); and prepared them for what to expect from specialist or hospital care (3.6%). Moreover, 3% reported they could access GPs on the phone (3.2%). Among patients sampled, only 2–4% of patients with a chronic disease were satisfied with the aforementioned aspects compared to 13–29% of patients without a chronic disease (p<0.0001).
Additionally, small percentages of participants reported that the GP listened to them (9%), helped them feel quick relief of their symptoms (10.7%), and feel better so that they could perform their normal daily activities (11.8%). Among patients sampled, only 7–10% of patients with a chronic disease were satisfied with the aforementioned aspects compared to 40–53% of patients without a chronic disease (p<0.0001). Furthermore, on average, only 4% of patients with a chronic disease reported being satisfied with the aspects examined in the clinical behavior domain, compared to 27% of patients without a chronic disease.
Table 3: Participant experience assessment by ‘clinical behavior’ of primary care domain overall and according to presence of chronic disease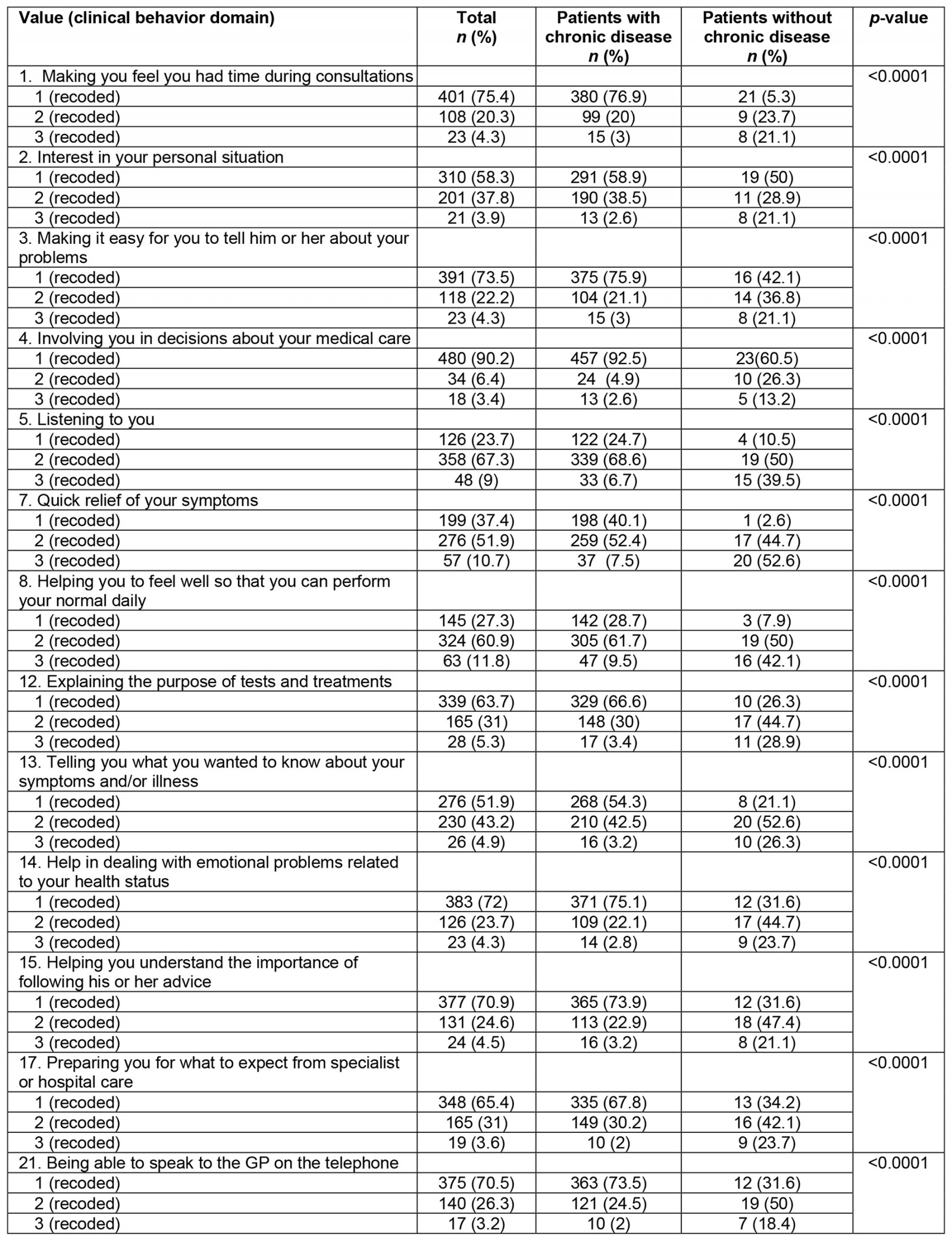
Support and services
Almost 12% of participants felt very satisfied with the GP’s thoroughness of the consultation (11.7%), physical examination (10%), and services offered for preventing diseases (9%). Among recruited patients, only 7–10% of patients with a chronic disease were satisfied with the aforementioned aspects compared to 34–40% of patients without a chronic disease (p<0.0001). Moreover, among patients with and without a chronic disease, a statistically significant difference was found regarding data confidentiality (32.8% compared to 57.9%, p<0.01). In contrast, there was no significant difference regarding the provision of quick services for urgent health problems (p=0.292). On average, 18% of sampled patients with a chronic disease reported being satisfied with the support and services provided, compared to 38% of patients without a chronic disease.
Table 4: Participant experience assessment by ‘support and services’ of primary care domain overall and according to presence of chronic disease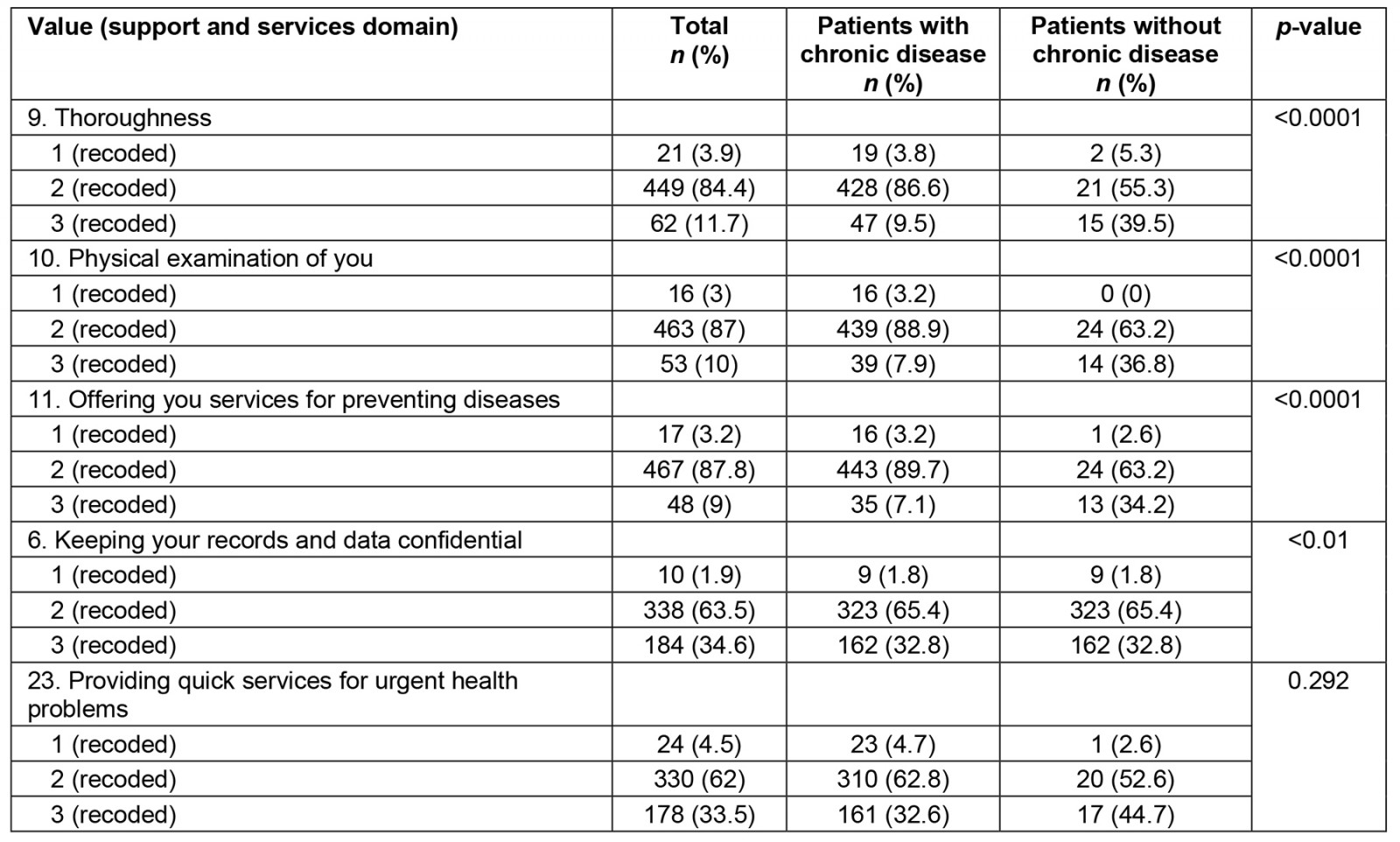
Organization of care
On average 3% of participants felt satisfied with organization of care aspects under consideration. Specifically, 3.2% felt satisfied with the helpfulness of other medical staff (except the GP), 4.1% with the waiting time (in the waiting room), and 2.8% with either getting through to the practice on the phone or getting a suitable appointment. Among recruited patients, 2.1% (on average) of patients with a chronic disease were satisfied with the aforementioned aspects compared to 18.4% of patients without a chronic disease (p<0.0001).
Table 5: Participant experience assessment by ‘organization of care’ of primary care domain overall and according to presence of chronic disease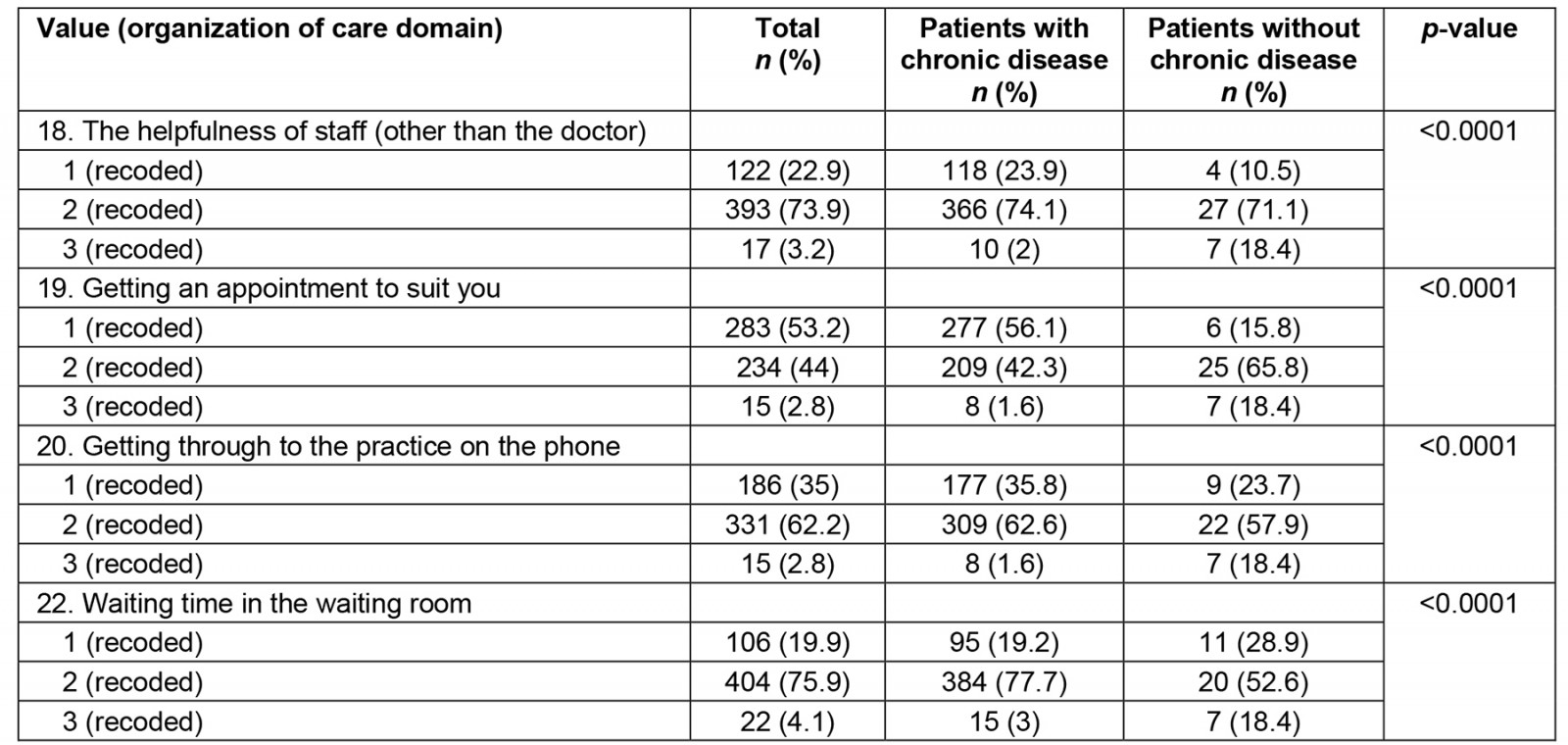
Discussion
Main findings and discussion in light of the literature
The study’s findings support that the organization of care domain is of highest importance and priority, while ‘clinical behavior’ and ‘support and services’ follow closely, as indicated by patient experience ratings (Table 6).
Over the past decade, healthcare providers and policymakers have recognized the importance of involving patients in improving quality of life and health13. Moreover, in recent years, organizational aspects of care, including responsiveness to patient needs, have received significant attention14. Similar to other studies, this study found that this aspect had the lowest satisfaction rating15-19. During the study period, PHC services in the public sector that served rural settings in Greece typically did not offer appointment bookings20, which may explain the reported wait times in this evaluation21. Wait times in PHC centers serve as significant quality indicators22 and underscore the need to improve this aspect of the Greek PHC system.
Regarding clinical behavior, the aspect of ‘the doctor listening to you’ aligns with findings in the literature15,17,23, where patients consistently give the highest positive ratings. Notably, while patients with chronic diseases valued aspects like ‘the doctor makes me feel better for daily activities’ and ‘the doctor provides quick relief’, patients without chronic diseases rated these aspects as less important. Effective communication skills and practices, essential for facilitating patient involvement in decisions about their health, are a crucial component of the clinical behavior domain. In our study, ‘patient involvement in decisions about their medical care’ received the lowest ratings, with no statistically significant difference between patients with and without chronic diseases. Communication skills, practices, and behavioral change skills seem to need more attention for an efficient PHC model. Lionis et al (2017) highlighted the challenges facing the Greek healthcare system as perceived by patients, emphasizing the urgency of continued efforts to improve person-focused primary care dimensions, including patient-centeredness, accessibility, continuity, patient involvement, comprehensiveness, and doctor–patient communication24. Communication skills and practices appear to be challenging aspects for the new PHC reform in Greece, and a renewed focus on delivering care to patients (particularly the quality of doctor–patient communication) may be an essential step in providing health care that genuinely meets patient expectations14.
The study also reveals that patients rated most items related to the support and services dimension with a score of 3 on the Likert scale, indicating that they were neither satisfied nor dissatisfied with the quality of support and services provided. Findings regarding aspects like ‘the doctor offers me services for preventing diseases’ and ‘the doctor is thorough during consultation’ broadly align with other literature data on patient evaluations of their care15,16,25-27. Patients without chronic conditions rated these items significantly higher than individuals with chronic conditions. Overall, this study indicates that, in the post-crisis period, patients were generally dissatisfied or neutral with most aspects of PHC delivery. The average percentages of patients providing positive evaluations of PHC provision (with answers 4 or 5 on the five-point Likert scale) were the lowest observed.
Table 6: Aspects related to primary healthcare delivery (for each dimension) ranked to be prioritized (based on positive patient experience rating) overall and according to presence of chronic disease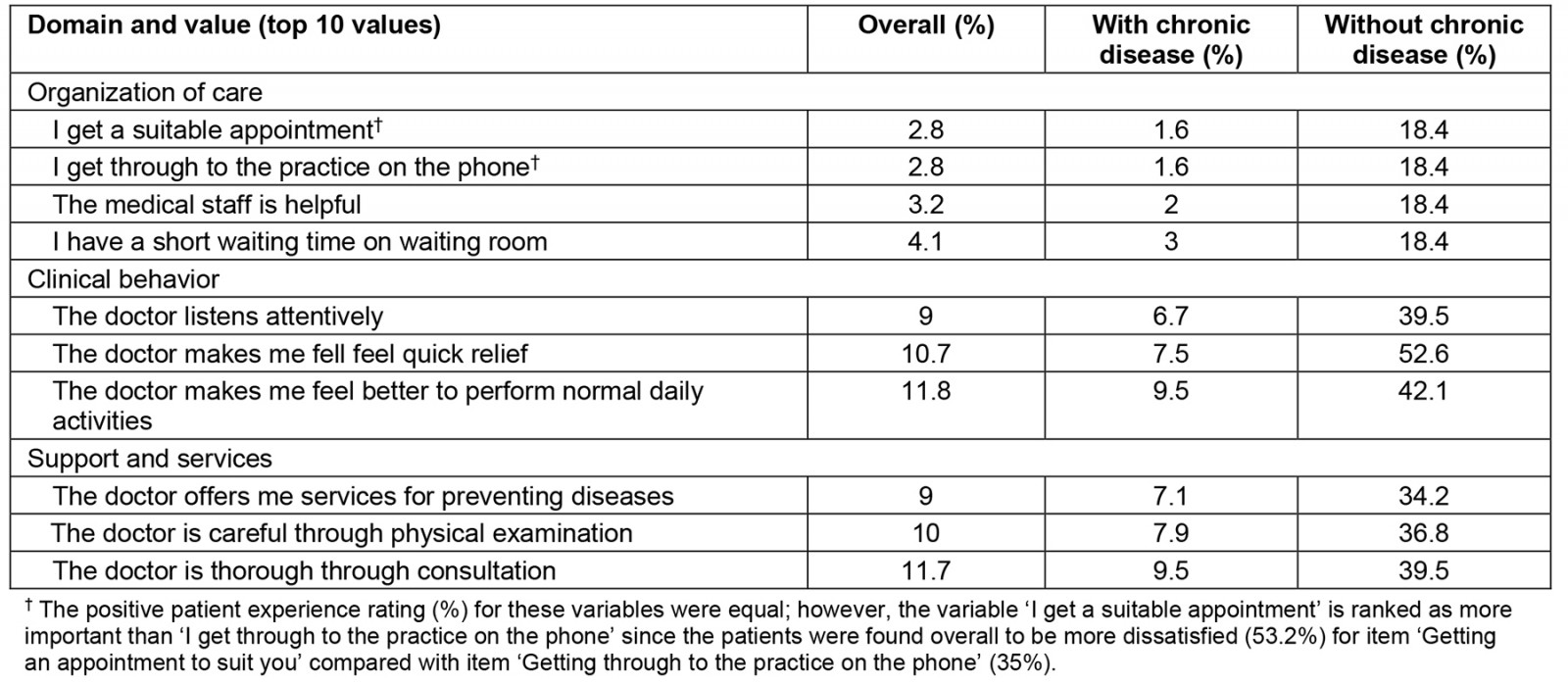
Limitations and future research directions
These study’s findings should be interpreted in the context of certain limitations. The primary limitation is the lack of generalizability of results since patients were recruited from one health region (Epirus) in Greece, mainly serving the rural population, while Greece comprises seven health regions. Consequently, the results cannot be extrapolated to the entire nation or the primary care population, especially those served by primary care units established in urban settings in recent years. Future work should explore how socioeconomic indicators and inherent geographical variations in healthcare infrastructure may affect the views, expectations, and perceptions of PHC attendees9. Additionally, this study cannot establish cause-and-effect relationships; for instance, patients who rated ‘clinical behavior’ poorly might also report low levels of communication with their GPs. The cross-sectional nature of the study limits examination to the effects of a single consultation, excluding previous interactions between patients and doctors. Furthermore, only univariate comparisons were performed for patients with and without chronic disease. In this way, we quantified how the existence of a chronic disease differentiates patient expectations, satisfaction, and evaluation of general practice services in rural healthcare centers in Greece. However, since most respondents in our study have a chronic disease, it may be of interest for future research to adopt multivariate statistical methods to explore the joint behavior of variables under consideration, identify potential confounders (such as self-reported health status, age, education level), and quantify the ‘clear’ impact of chronic diseases in this context.
Another limitation is that the study's data collection occurred before the pandemic, and its impact on the quality of PHC services remains unknown. Moreover, the suitability of the study population (first utilized for validation purposes) for the current health policy analysis depends on various factors. While a validation study focuses on assessing the accuracy and reliability of a certain measurement tool test within a specific population, a health policy analysis paper typically aims to evaluate the effectiveness, implications, or outcomes of health policies (and/or interventions) within a broader context. The research objectives of the current article, the nature of the previous validation study9, and the relevance of the population to the health policy being analyzed are three key factors ensuring that the study population utilized here aligns satisfactorily with the requirements and focus of this health policy analysis paper. Finally, although EUROPEP was previously found to be robust for exploring patient views and changes over time in different economic contexts9, all insights here are derived from one observation-based assessment tool.
Based on the research outcomes and considering the extracted scores for all aspects of each domain, future work could aim to provide a deeper understanding of patient evaluations of care (both in general and in specific aspects) to answer the key question, ‘What do generally good or poor patient assessments mean, and how do they reflect optimal care and outcomes?’ Howie et al (1998) noted that components assessing patient satisfaction with a consultation often reflect their expectations rather than the actual benefits derived from it28-30. However, it could be argued that practice and patient evaluations of their GPs are important care outcomes, although they need to be considered alongside other outcomes.
Implications for practice and policy
This study offers insights into what patients expect and value in general practice care, emphasizing factors that may shape the successful implementation and outcomes of Greek public PHC reform, particularly the personal doctor initiative. The findings include elements closely aligned with the new personal doctor tasks and highlight aspects within the PHC system that patients consider crucial for prioritizing quality improvement efforts to strengthen PHC delivery in Greece.
The concept of personal doctor services might be translated and adapted to a rural environment by enabling the role of a community doctor. A community doctor can assist families and their members in a personalized manner. Geographical settings with less than 2000 inhabitants might represent an already existing source of registration. Home visits within a limited spatial area, in combination with supportive applications and telemedicine tools31, can balance the eventual access gap that affects rural areas. Focusing on the fields that EUROPEP revealed as weak aspects of patient satisfaction, it is conceivable that issues such as time spent during consultations, interest in personal situations, helpfulness with personal problems, concerns and emotional matters related to health status might be improved overall. Getting through to a rural practice on the phone, as well as getting a suitable appointment, are details that can be discussed with user-friendly apps (easy for patients to use) and a good relationship between doctor and patient. Providing comprehensive preventive care and helping patients monitor chronic conditions are essential for improving service delivery tailored to this population. Community doctors can link patients' geographical, linguistic, socioeconomic and cultural peculiarities with the local health source.
This concept is important to be discussed as the European Union is a body of countries with many differences and organizational diversity. With much institutional compactness, but with a lesser functional readiness, each country and part of a country should learn to liberally organize its services32 in order to satisfy general directives and local needs. To support this dual scope, health systems need tools and monitoring mechanisms. Models or solutions from other countries cannot be transferred to others without knowing current local weaknesses and without suggesting adaptations.
Research that could test variables on behavioral and daily habit aspects within living in rural and remote environments, to be combined with healthcare delivery and outcomes, deserves a fresh and alternative conceptual approach. Rural health research can invest in a mix of advanced methodologies, from controlled to quasi-RCT trials, but with the spirit of real-world studies in order to not lose influential trends of a different way of living33.
Considering our findings and guided by the law establishing the personal doctor as the primary contact within the Greek health system, several person-centered and PHC-centered actions are recommended to achieve universal health coverage and enhance the role of the personal doctor. These recommendations encompass three key directions: patient level, practitioner or professional level, and decision-making and organizational levels.
At the patient level, the results of this study convey important messages about patient priorities in general practice and areas for potential quality improvement. Policymakers could consider steps such as implementing more effective interventions targeting patients as part of the national primary care system. These interventions might include person-centered consultations, improved accessibility, transitions, and continuity of care34, patient education, feedback collection from patients, patient access to records, and the utilization of support tools and technology35. Furthermore, it is valuable for GPs to be informed about their patient evaluations, allowing them to identify opportunities for improving personal care or practice organization. Patient satisfaction, as a quality component, underscores the importance of communication and empathy, access, and involvement in future conceptualizations of quality in general practice. Strengthening PHC following a multidisciplinary approach could address the various subgroups within the population, focusing on meeting people's healthcare needs on their terms.
At the practitioner or professional level, rather than assuming that professionals automatically possess the skills for improvement, specific training in quality improvement for general practice teams should be intensified35. Training programs that involve GPs in more patient-centered communication have been shown to enhance patient compliance and outcomes36. The results of this study suggest that policymakers need to continue their efforts to improve PHC services by adopting effective interventions targeting professionals, including training in quality improvement methods, collaborative learning among health professionals, audit and feedback, educational outreach visits, joint initiatives, decision support tools, and increased staffing levels35. Furthermore, medical schools and universities in Greece could prioritize patient-centered care in continuing medical education programs and other healthcare professional education programs37,38, as well as university school curricula22,24.
In terms of the decision-making process, especially with the introduction of the PHC reform in Greece, strategies for promoting patient-centered care, such as shared decision-making, need to be explored, particularly among vulnerable groups. Results from studies focused on patient health needs and the survey's agenda related to evaluating the quality of services provided can be used to inform decision-making processes. In the context of the current reform, especially with the development of new local health units37, information on patient priorities can be precious39. Other European countries facing similar challenges within their PHC systems could benefit from considering these research findings.
Finally, at the practices and organizational level, quality improvement efforts in primary care are closely linked to organizational issues and the process of care provision, such as integrated primary care delivery and technology (eg e-health)40,41. Policymakers need to continue their efforts to enhance PHC services through interventions at the practice level, including quality improvement projects, telecare37, guideline implementation, clinical audits, electronic medical records, improved data collection and analysis, and error reporting35.
Conclusion
This article highlights the factors that may shape the effective implementation and outcomes of Greek public PHC reform and recommends them for evaluating the personal doctor initiative to serve both rural and urban area. Aspects of EUROPEP related to the personal doctors’ new tasks, as perceived by patients, can be used to prioritize quality improvement activities to strengthen PHC delivery in Greece. This article also contributes to the evolving knowledge base for developing more person-centered approaches in modern medical practice. When policymakers seek to address significant financial challenges, they need to implement human-centered approaches that stimulate a more efficient system of high-quality health care, emphasizing the importance of human dignity and moral values. Although the key messages of this study are derived from rural settings and reflect a pre-pandemic context, they remain relevant.
Acknowledgement
The authors would like to thank the GPs, the many patients, and the medical staff at PHC centers of Epirus in Greece for their contributions to this study.
Funding
This research received no external funding.
Conflicts of interest
The authors declare no conflicts of interest.
References
You might also be interested in:
2015 - Effect of rural practice observation on the anxiety of medical students
2008 - Quality of life in patients with sickle cell disease in Jamaica: rural-urban differences


