Introduction
Injury from trauma is the leading cause of death in Australia for people aged 1–44 years1. Death from trauma is most likely to occur within the first hour of an incident; however, many fatalities are preventable if efficient and effective care are provided2,3. Unfortunately, rural and remote areas face greater time, distance and resource constraints in providing emergency care, and subsequently experience higher rates of morbidity and mortality than urban settings4-6. In the state of Queensland, Australia, approximately 40% of the five million residents live in rural and remote areas that span across 1.7 million square kilometres7,8. Although the vast Queensland landscape cannot be changed, individual hospitals and health services can ensure that clinicians are equipped with the knowledge, tools and skills to successfully manage these emergency conditions as efficiently as possible.
In Queensland, each of the 16 hospitals and health services are responsible for developing and delivering their local trauma resources. However, limited communication and collaboration across the vast service areas often means individual facilities develop and deliver their own trauma education programs or outsource the work to external organisations. This produces inconsistencies in the content, processes, volume and regularity of trauma education provided across facilities, ranging from no training to full-day annual workshops. Rural and remote facilities are most disadvantaged by this unstandardised structure because they have fewer resources available for training and education and are less physically accessible than tertiary facilities.
Training needs
Queensland’s Clinical Skills Development Service (CSDS) and the Jamieson Trauma Institute (JTI) conducted a training needs analysis (TNA) to quantify the gaps and opportunities in the development and delivery of trauma care education throughout Queensland Health. The TNA involved extensive stakeholder engagement, including nursing and medical staff working in emergency departments, and clinicians from rural, regional, and tertiary hospital facilities across Queensland. Stakeholders were engaged about current training gaps, challenges and barriers to effective trauma education, and training and educational needs moving forward. The TNA also involved a review of currently available trauma education courses and resources throughout Australia, including their focus area, target audience, length and costs associated. The outcomes from the TNA revealed both key barriers to success and multiple training needs to improve the provision and uptake of effective trauma care education, particularly in rural and remote settings. The TNA outcomes are presented in Table 1.
To address these barriers and training needs, the CSDS, JTI and Queensland Trauma Clinical Network (QTCN, previously the Statewide Trauma Clinical Network) created the Queensland Trauma Education (QTE) program in 2021. QTE was established to complement, not replace, available trauma courses and resources. The aim of this article is to review the QTE program and assess the benefits to clinicians in both the delivery of education and the provision of trauma care.
Table 1: Key barriers and core training needs identified for effective trauma education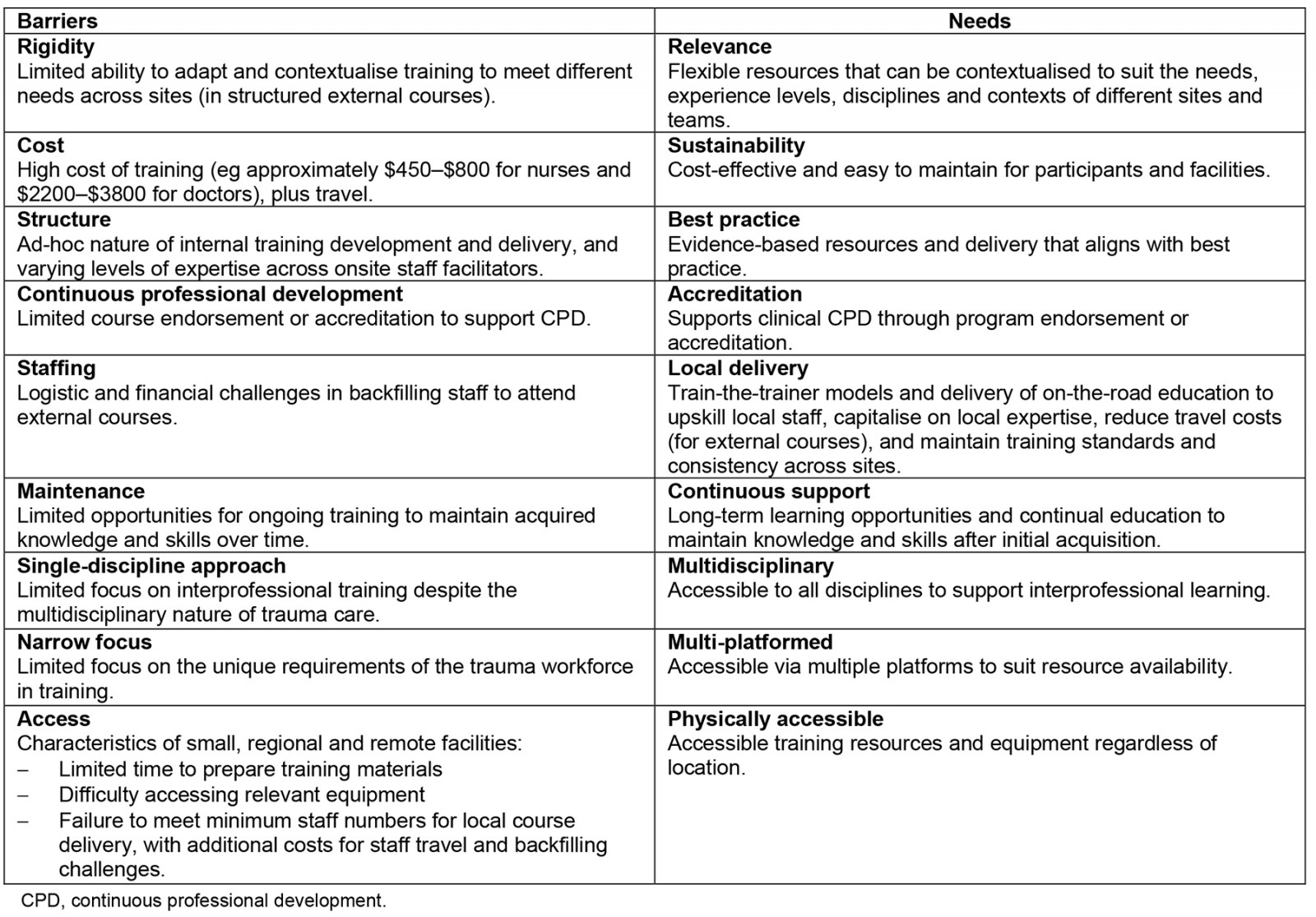
Methods
Intervention
The QTE program was developed using an iterative design process, including regular consultation with subject-matter experts from both trauma care and clinical education fields. Subject-matter experts were responsible for the creation, review and iterative revision of program materials. Learning theories relating to interprofessional education, peer-based learning, deliberate practice and experiential learning were used as the foundation for the development of the simulation-based learning program9-13. QTE comprises a full-day face-to-face simulation course and a separate online platform of extensive trauma care tools and content, including modular training resource kits, clinical guidelines and clinical resources (eg assessment tools, flowcharts, videos, cognitive aids). QTE resources are all freely available at https://csds.qld.edu.au/qte. QTE is further supported by the CSDS Pocket Centre Network (PCN; https://csds.qld.edu.au/pocket-centre-network), a network providing access to and delivery of high-quality simulation equipment to support onsite training and education across Queensland Health facilities.
Evaluation
The RE-AIM (Reach, Effectiveness, Adoption, Implementation, and Maintenance) framework was used as a guide to evaluate the QTE program14. A mix of qualitative and quantitative measures were used to review the program against each element of the RE-AIM framework and to assess its alignment with the needs identified in the TNA. The review involved auditing the online platform (QTE website) and capturing data relating to use and access of online tools and resources, location of users, user feedback on website resources, number of face-to-face courses completed, course locations, number of participants, form of training provided (ie internal to CSDS, on-the-road, train-the-trainer), and the equipment provided through the PCN. Face-to-face courses were further assessed using data obtained through a pre-course survey and a post-course survey.
The pre-course survey included questions regarding the participant’s background (eg professional discipline, experience level, location, reason for doing the course) to allow for course adaption of content, structure and activities to suit attendees. The post-course survey included multiple-choice and open-ended questions regarding course satisfaction, value of simulation equipment, scenarios and activities, application of knowledge to practice, quality of facilitation, quality of feedback obtained, most valuable and least valuable elements of the course, and other areas of trauma education required or of interest. The measures and findings presented in this report reflect the data collected between the QTE pilot in April 2021 and September 2023. However, QTE is a continuing program with ongoing data collection and iterative quality improvement changes that may not be captured in this report. The RE-AIM model was contextualised to suit the aims and scope of this evaluation, with all measures presented in Table 2.
Ethics approval
This project was an internal quality improvement pilot and did not require formal ethical review. However, this work adhered to all relevant ethical conduct standards and the SQUIRE V.2.0 guidelines were followed in preparing the manuscript15.
Results
A summary of the data analysed from QTE face-to-face courses and website resources is presented using a RE-AIM framework in Table 2.
Table 2: Evaluation of QTE using the RE-AIM framework and alignment with TNA outcomes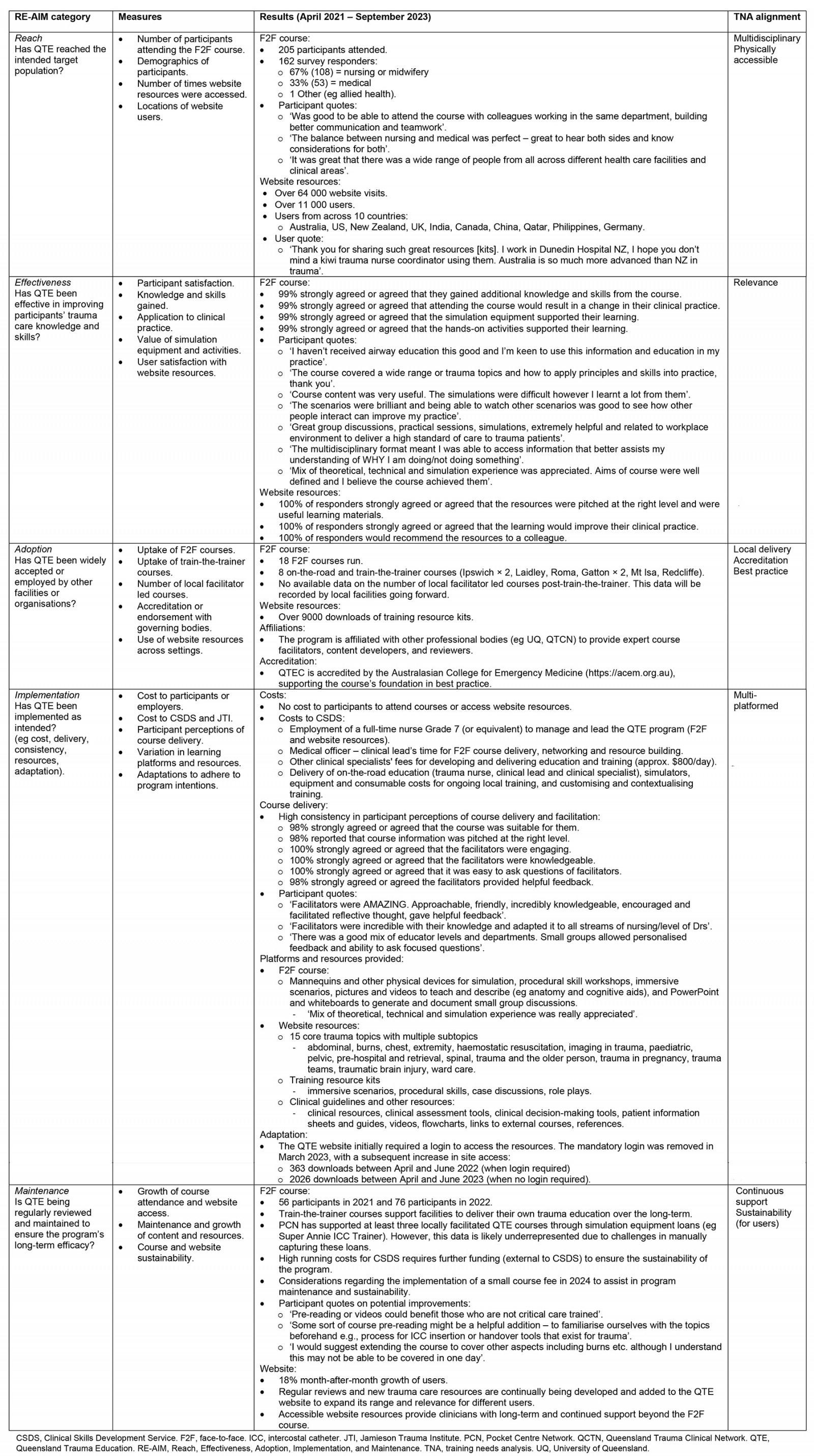
Discussion
Overview
The findings of this review demonstrate the reach and effectiveness of QTE, where barriers and challenges remain, and where lessons have been learnt to inform future statewide education. Overall, the analysis demonstrates how QTE aligns with the original training needs identified. Alignment is evident in the variety of content and the flexibility of resources available to suit different clinical disciplines, experience levels, contexts, training platforms and needs. The program materials support onsite continuous education, including free train-the-trainer and on-the-road courses, open access to online training resources, and use of simulation equipment available through the PCN, which further highlight QTE’s sustainability and accessibility. Accreditation and affiliations with multiple professional bodies also demonstrate QTE’s robust evidence base and use of best practice.
Beyond the alignment with identified training needs, the program has been successful in reaching the target population (ie clinicians delivering or providing trauma care). This is evident in both course and website data, with over 200 clinicians from nursing, midwifery and medicine participating in face-to-face courses, and over 11,000 users of online resources. QTE has also been effective in improving trauma knowledge and skills, with 99% of course participants and online users agreeing that QTE supported their learning and would result in a change in clinical practice. QTE’s endorsement by and affiliation with other relevant organisations (eg ACEM accreditation) further highlights the program's wider adoption and acceptance. Moreover, the program has been successfully implemented in line with initial intentions, including effective course delivery, free access and use of multiple learning platforms. QTE has also been maintained and adapted effectively over the longer term, with continuous growth in resources and clinician access.
Limitations
Despite the benefits, further work is required. First, engagement with other disciplines that encounter trauma scenarios (eg allied health, paramedics) has been limited, despite the program being available to all specialties. Increased engagement with other professional and non-professional streams is required to improve awareness of, and access to, QTE. The current data are limited to self-report measures to assess QTE’s efficacy, rather than the measurement of objective performance. However, any changes in participants’ trauma care performance post-QTE could be confounded by differences in location, time between training, trauma exposure, team size and availability of resources. To address this challenge, case studies of single sites (with case-matched controls) that have not yet received any QTE training are being planned.
Data relating to equipment usage and local facilitation of QTE courses (post-train-the-trainer) relies on manual input across facilities with varying processes, resources and constraints. This manual and unregulated process can produce discrepancies and omissions in reporting, as highlighted in the ‘Maintenance’ section of Table 2. Clearer reporting structures and more automated processes are subsequently required to ensure reliable and accurate data are collected going forward.
In addition, this review demonstrates how QTE provides a more sustainable training model for clinicians and facilities. However, sustainability challenges remain for CSDS and JTI. The high costs and resources associated with the continuous development and delivery of a growing QTE require external funding or changes in the cost structure to ensure the longevity and value of the program. Moreover, any changes in fee structure need to be weighed against the impact on accessibility.
Lessons learned
Beyond the challenges involved, several learning opportunities were identified throughout the evaluation process. For example, a mandatory login was originally required to access QTE’s online training resources. While the login enabled the collection of additional user data, course developers questioned its potential impact on resource accessibility. When the mandatory login was removed, downloads increased by 550% compared to the same period the year prior (when a log-in was required). This substantial increase in downloads highlights that even simple steps and tasks can impede the reach and accessibility of online resources and should always be considered during implementation and maintenance.
Additional opportunities for innovation were identified throughout regular reviews of participant, facilitator and subject-matter expert feedback, resulting in changes to the structure, content and platforms available. For example, participant feedback has led to the introduction of pre-reading materials to further scaffold and space learning, the development of a guide to assist users in the selection of relevant online resources to suit their unique training needs, and the continuous development of new trauma topics to expand QTE’s accessibility and relevance. Moreover, participant feedback firmly reiterates the value of QTE’s interprofessional approach to training, not only for improved technical skills in trauma management, but also for enhanced teamwork, communication and compassion. These variables can all significantly impact performance in emergency scenarios and may encourage further considerations of local system improvements16.
Conclusion
Overall, QTE has been successful in improving the quality of trauma care education across Queensland. Although further work is required to ensure the long-term sustainability of the program’s delivery, QTE provides clinicians with the necessary tools and resources to increase their trauma management skills and improve patient outcomes. QTE further supports healthcare workers based in rural and remote facilities by providing resources that are both accessible and relevant across geographically challenging landscapes.
Acknowledgements
Thank you to Kimberley Ballinger, Tracey McLean and Luke Wainwright for their input into QTE at the CSDS.
Funding
Authors LO and FW were funded by the CSDS and JTI to develop and deliver educational materials for the QTE program under the guidance of Author BF, Nursing Director of CSDS.
Conflicts of interest
Authors KM and MM led this internal quality improvement review as employees of the CSDS, but were not involved in development, delivery or administration of the QTE program. No other competing interests are declared.
References
You might also be interested in:
2018 - Pre-graduating medical students' interest in rural internship
2013 - Comment: Inter-Island referrals in Solomon Islands: a remote hospital perspective


