Introduction
Despite the existence of numerous evidence-based psychosocial treatments, access to these treatments is quite limited1. Most people with mental health conditions do not seek treatment or do so only after living with the condition for years2. When treatment is sought, what is provided often falls short of the minimum standards suggested for adequate care3. As daunting as these challenges are to accessing quality treatment, they are felt even more acutely in rural areas where access to care is more limited4, leading those in more rural communities to often rely on informal care, including support from friends and family members5.
Obstacles to rural mental health care
Rural areas face many challenges that complicate access to care. Among the greatest barriers is the dearth of mental healthcare providers4,5. Socioeconomic disadvantages and a lack of occupational opportunities lead to relatively few mental health service locations in rural areas6. Many rural counties lack a psychiatrist or master’s level social worker5. Those in more rural areas are also more likely to rely on a primary care provider for mental health treatment, and even when psychotherapy is received it tends to be in a smaller dose than in urban areas7.
An additional obstacle related to this lack of providers is that those in more rural areas often need to travel longer distances to access treatment, which also exacerbates the financial costs of seeking treatment4. Another obstacle is that those in rural areas less often have employer-sponsored insurance plans and more frequently rely on public services, which remain severely limited4,5,8. Compounding the problems of limited availability are the problems related to mental health being stigmatized, a particular problem in rural areas4,9. In fact, evidence suggests those in rural areas are both less likely to seek treatment and less likely to recommend treatment to a loved one5.
Models of informal care
Given the barriers to formal care, informal care is more common in rural areas5. Nonetheless, those with a loved one struggling with mental illness may not have the understanding or special skills that would be useful in providing effective support and encouragement. Instead, psychosocial interventions for mental health conditions largely comprise interventions focused almost exclusively on the individuals with the conditions. The most common treatment formats are standard face-to-face individual psychotherapy and group psychotherapy in which one or small groups of patients are treated by one or two treatment providers10. Such treatments are expensive and difficult to provide on a large scale1, and thus fall far short of meeting the needs of those in rural areas. Additionally, providing informal care can itself increase psychological distress, especially when such care is relied on frequently11-14. An intervention that teaches evidence-based coping skills for use with individual mental health concerns and to facilitate providing informal care would thus be consistent with the needs of those in rural areas.
Some research has examined the benefits of interventions provided to people who are important in the lives of those with mental health concerns. In one example of a treatment aimed at developing more positive communication patterns among family members, family focused treatment for bipolar disorder has been found to reduce the risk of relapse15. Similarly, behavioral marital therapy, which includes an intimate partner in treatment, is an effective treatment for depression16. Another intervention developed to impact the lives of those in treatment for mental illness by intervening with their social networks is a program called Family Connections, for family members of those with borderline personality disorder17. The program was developed to teach coping skills and provide social support, and has been found to reduce the psychological symptoms of caregivers and improve coping skills17. Although these programs indicate some attention to intervening with the family and friends of those receiving treatment for specific mental health problems, this strategy has seen very limited use and, to our knowledge, has yet to be developed for use in rural communities specifically.
In considering strategies that may be beneficial for informal caregivers, we focus on cognitive behavioral therapy (CBT) skills, a set of strategies with considerable support in the management of individual mental health concerns18. CBT skills refer to the broad set of strategies clients learn in CBT. Cognitive restructuring and behavioral activation skills are focal to CBT, but CBT skills can also include other strategies a broadly trained CBT therapist might seek to foster, including interpersonal and mindfulness/acceptance skills19. Clients’ improving knowledge of and use of CBT skills have been found to characterize more successful courses of treatment and outcomes that are more enduring20, and a growing body of evidence further indicates that learning CBT skills has benefits outside the context of treatment, including among caregivers18. However, to our knowledge, an intervention package drawing on these strategies that attends to the unique challenges faced by informal caregivers in rural areas has yet to be developed.
In this study, we pilot-tested the Friends and Family for Mental Health program, a CBT skills-based intervention aimed at teaching evidence-based CBT to those providing informal care in rural communities. The stress related to providing informal care can itself contribute to mental health concerns. Thus, this program focuses on both providing participants with skills that can be useful in providing informal care and managing their own mental health symptoms. We believe this approach is well suited to the rural context, in consideration of the greater reliance on informal care in these areas5.
We had two primary goals for this initial open, uncontrolled pilot study. First, we planned to provide an initial test of the benefits of the program. Our primary focus was change in informal care skills from baseline to follow-up. In addition, we assessed change in hope, psychological symptoms, and CBT skills from baseline to a 1-month follow-up assessment. We hypothesized the program would enhance participants’ informal caregiving skills. As the program draws on strategies supported for treating individual mental health concerns, we also anticipated reductions in psychological symptoms. We further anticipated improvements to the psychological resources of participants, as indexed by hope and CBT skills. The second goal of this study was to collect participant feedback to inform further development of the program. To do so, we evaluated participant views concerning the credibility of the program and included additional questions immediately following the program to collect overall feedback and to determine participant preferences for different program components.
Methods
Participants
Participants were 37 adults who resided in a rural county of Ohio in the US at the time of the study. To be eligible, potential participants had to meet the following inclusion criteria: (1) be aged 18 years or more, (2) reside in a rural county in Ohio as indicated by self-reported rural resident status and ZIP code, (3) have access to a reliable internet connection and (4) indicate interest in participating in the program to better support friends and family. Of an initial 63 individuals who expressed interest in the study by responding to a pre-screening survey, four individuals were not invited to participate due to residence in a non-rural county, and one individual was not invited due to residing outside of Ohio. Of the 58 who were invited to participate in the pre-intervention survey, 37 did so and all 37 went on to participate in a skills group and the subsequent post-intervention survey. All but one participant completed the follow-up survey 1 month later.
We defined ‘rural’ using the Office of Management and Budget definition, which defines rural areas as those that are not part of a metropolitan statistical area21. All participants answered ‘yes’ to a question asking whether they resided in a rural area, and reported a county of residence for which the rural status was corroborated. The counties represented in the sample are shown in Figure 1.
Although we made no deliberate effort to recruit men and women differentially, a striking feature of our sample is that almost all participants identified as male (94%; n=35). The mean age of the sample was 29 (standard deviation (SD)=4.8, range=21–50). Most participants identified as White (68%; n=25), with 30% of participants identifying as Black/African American (n=11) and one participant preferring not to answer. Slightly less than half of participants reported having completed a graduate or professional degree (44%; n=16), with some participants working towards a graduate or professional degree (22%; n=8), some participants reporting a 4-year degree as their highest attained degree (33%; n=12) and one participant preferring not to answer. Most participants were currently married or cohabitating (95%; n=35). A very high proportion of participants had at least one child (89%; n=33), and over half of participants reported a household size of four or greater (76%; n=28). No participants reported current participation in psychological treatment at the time of the study. The study utilized four attention checks (three in the pre-intervention survey and one in the follow-up survey). All participants passed at least one of these checks (ie reported the correct response to at least one attention check question), and 97% (n=36) of participants passed all attention checks.
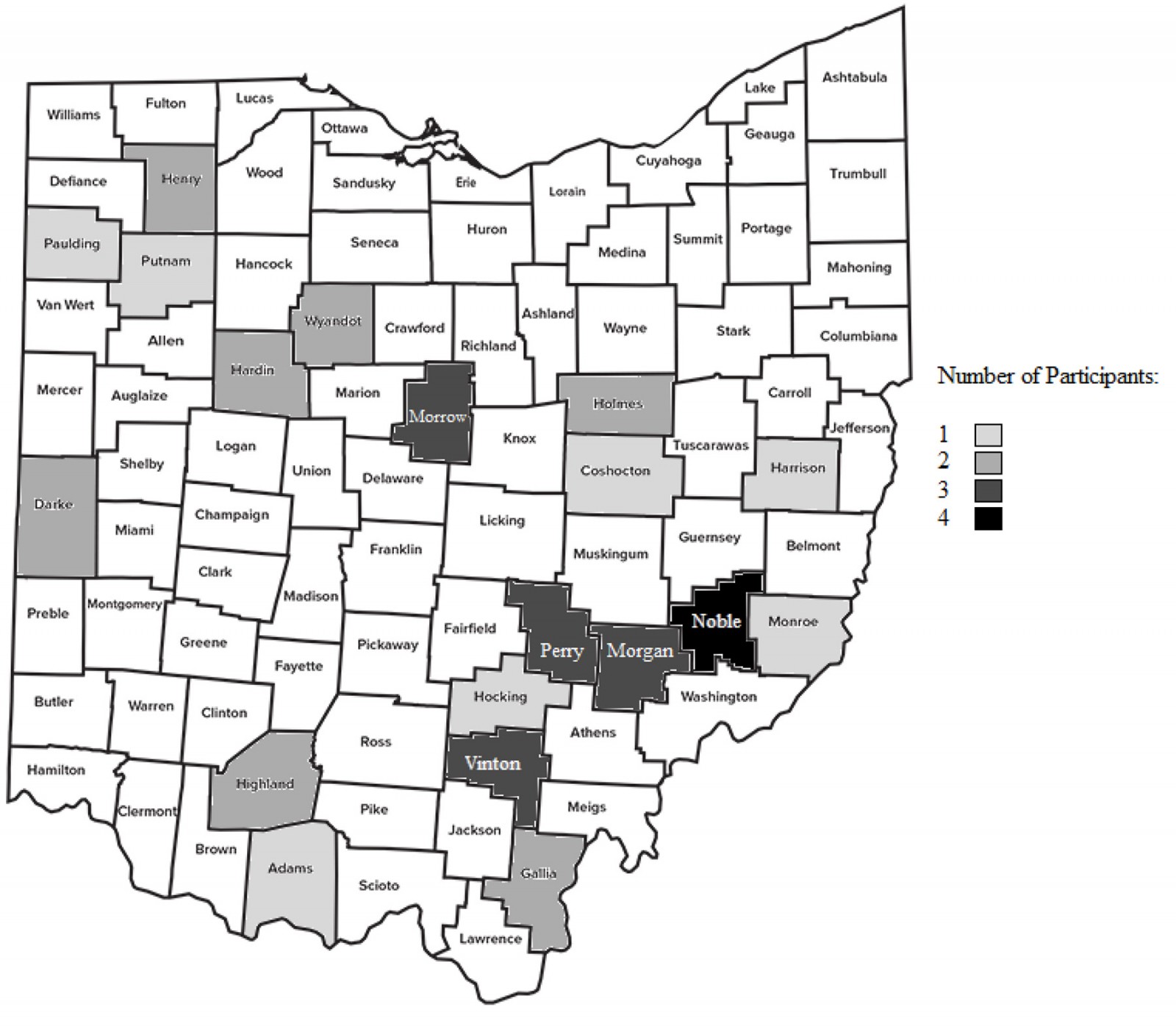 Figure 1: Ohio county representation in study sample.
Figure 1: Ohio county representation in study sample.
Recruitment
Participants were recruited using free advertisements in newspapers servicing rural counties and mental health resource list-serves targeted at those in rural communities. The program was described as a free mental health skills program that would provide training in different types of coping skills and problem-solving strategies that have been effective at treating individual mental health concerns. These advertisements also stated that the program would focus on teaching ways these strategies could be used when providing support for friends and family members struggling with mental health concerns. Advertisements directed those interested in participating to a study webpage that included a description of the study and link to a screening survey. The study website included the same description as the study advertisement, in addition to listing the inclusion criteria for the study, the study incentives (a $15 Amazon gift card for responding to the post-intervention survey and a $15 Amazon gift card for responding to the follow-up survey), and the length of the program (1 hour and 15 minutes). The screening survey asked participants to report information relevant to eligibility criteria and provided times the program would be held, asking participants to indicate the time they would prefer to participate in the program. Two separate mental health skills groups were held, one with 14 (38%) participants and the other with 23 (62%) participants. Both programs were led by the same two hosts (the first and third authors of this study).
Intervention
The Friends and Family for Mental Health Program is a mental health skills training program developed by this study’s authors. This intervention broadly draws on strategies from various forms of CBT22-24, focusing on cognitive, behavioral, and interpersonal skills. The program also included psychoeducation on common mental health concerns and evidence-based mental health treatments. The program utilized a webinar style with use of a slide deck. Two hosts shared their videos and discussed slides, and participants had the option of remaining anonymous or contributing to the webinar chat. The program started with psychoeducation on common mental health concerns and the benefits of psychological treatment. The benefits of goal setting were then emphasized, and participants were encouraged to set several short- and long-term goals and consider the use of program strategies to pursue those goals. Behavioral strategies were then described, including self-monitoring, activity scheduling, structuring, and counteracting avoidance. Participants also received psychoeducation on mood-dependent behavior. Cognitive strategies were then discussed, beginning with psychoeducation on negative automatic thoughts and the cognitive triad23. Identifying thoughts and feelings, distancing, weighing evidence, and identifying alternative perspectives were discussed. This also included discussion of how to use a thought record, and thought record examples were used to demonstrate the benefits of cognitive restructuring. Interpersonal skills were then discussed, including assertiveness skills and validation. Examples included use of these strategies for individual mental health concerns and in situations involving friends and family members. The importance of continued practice using CBT skills to facilitate skill development was then emphasized, and participants were encouraged to practice using the thought record and activity log on an ongoing basis.
We recognize that caregivers are at higher risk for mental health concerns11-13. Because there may be less stigma in seeking help as a caregiver than seeking personal support, we hoped the focus on caregivers would provide a welcoming context that allowed us to address both caregiving challenges and personal concerns. Insofar as this allowed those who might otherwise be put off by stigma to get some assistance, we regarded this as a positive feature of the program.
Materials
Credibility/Expectancy Questionnaire (CEQ): The original CEQ is a six-item questionnaire that measures participant attitudes regarding treatment25 but is frequently adapted for use with different treatment designs. In this study, we adapted the CEQ to utilize three items assessing participant views concerning how logical the program was, how successful the program would be in helping reduce distress, and how confident participants would be in recommending the program to a friend.
Generalized Anxiety Disorder Questionnaire-7 (GAD-7): The GAD-726 is a seven-item self-report measure of anxiety. Items are based on the diagnostic criteria for Generalized Anxiety Disorder (GAD) from the fourth edition of Diagnostic and statistical manual of mental disorders (DSM-IV)27. GAD-7 scores have good test–retest reliability and are related to other measures of anxiety symptoms26.
Patient Health Questionnaire (PHQ-9): The PHQ-928 is a self-report measure of depressive symptoms. Items are based on the diagnostic criteria for major depressive disorder from the DSM-IV. PHQ-9 total scores have good sensitivity and specificity for major depression and are related to other measures of depression symptoms28.
Styles of Emotion Regulation Questionnaire (SERQ): The SERQ19 has 72 items, using 36 item stems, each with two questions. Respondents are asked about their frequency of skills use and the extent to which being emotional negatively impacts their ability to use their skills. Factor analysis supports four skill factors (cognitive, behavioral, mindfulness, and interpersonal skills) and one emotionality factor19.
Trait Hope Scale (THS): The THS29 is an eight-item measure of hope. Participants respond indicating their agreement with statements reflecting agency and pathways. The agency subscale, which evaluates goal-directed self-determination; and pathways subscale, which evaluates planning to meet goals, each have four items. The THS subscales and total score have good internal consistency and construct validity29.
Program Impact Questionnaire: To assess how impactful the program would be in improving participants’ informal care skills when providing support to friends and family members, we used a novel set of five questions we created for this purpose. This set of questions asked about how the program might impact the participants’ most important informal caregiving relationship. These items used a scale of 1 (‘not at all’) to 5 (‘extensively’). The items were scored by taking the total score. The internal consistency for the small number of items making up this measure was modest (α=0.55).
Support Confidence Questionnaire: As another means of assessing informal caregiving skills, we assessed participant confidence with providing support to friends and family members using a set of six questions we created for this study. Items asked participants about their confidence in several behaviors related to providing support to friends and family members with mental health concerns, including discussing mental health, providing support, and discussing treatment. Items used a scale of 1 (‘not at all’) to 5 (‘extremely’) with regard to level of confidence. Items were scored by taking the sum of all items. The internal consistency for the small number of items making up this measure was modest (α=0.56).
Post-program handouts: After participating in the program, participants were emailed three handouts to facilitate continued use of the strategies described in the program, including a thought record, an activity log, and a skills card. To gain facility with the cognitive restructuring strategies during the program, participants worked through several examples of using thought records30. Participants were told they would be sent a blank thought record and were encouraged to use it in distressing situations. Participants were introduced to self-monitoring, structuring, and scheduling strategies by going over examples of activity logs30. Participants were instructed in ways to use the activity log to monitor behavior, and practiced evaluating and breaking down problems identified using the activity log. Participants were told they would be sent an activity log and were encouraged to use it in the pursuit of their own goals. Participants were also sent a document describing ways to use different CBT skills, referred to as a skills card31, which they were encouraged to draw from when in distressing situations. This document included descriptions of activity monitoring, structuring, activity scheduling, distancing, and cognitive restructuring.
Analytic strategy
To test intervention benefits for variables that were measured at all three time points (pre-intervention, post-intervention, and follow-up), we utilized repeated-measures analysis of variance (ANOVA) to compare differences at each time point. For significant effects, we compared mean differences with follow-up Student’s t-tests. For variables that were only assessed pre-intervention and at follow-up, we utilized paired-sample t-tests to evaluate differences. For additional feedback questions (given immediately following the program), we planned to examine descriptive statistics to inform our efforts to refine the program for future offerings.
Ethics approval
This study was approved by the Ohio State University Behavioral and Social Sciences Institutional Review Board (IRB number 2021B0251). Informed consent was obtained from all individual participants in this study.
Results
Feedback
To obtain program-specific feedback, we evaluated participant’s CEQ scores in addition to responses to prompts regarding the utility of the program. The mean CEQ score, reported following the intervention, was 23.05 (SD=1.97), reflecting an average score of 7.7 out of the nine-point range on each CEQ item, indicating the intervention was viewed as highly credible. Participants also responded to questions evaluating their attitudes towards psychological treatment generally and about the Friends and Family Program specifically. Results from feedback surveys are presented in Figures 2 and 3. As shown in Figure 2, participants reported finding the program helpful, with 84% reporting the program was at least very helpful. Participants also reported finding the program was relevant to them, with 89% of participants reporting the program was at least very relevant (Fig2). Participants were asked how likely they felt they were to use the strategies they learned in the program, with all but one participant indicating they were likely or extremely likely to do so (Fig2). All participants were at least moderately interested in a second workshop offering, and 81% of participants were at least very interested in a second offering.
General feedback regarding mental health resources is shown in Figure 3. As shown in Figure 3, ‘a few times a year’ and ‘monthly’ were the most common desired frequencies participants indicated would be of greatest interest to them for attending mental health skills programs, with each selected by 32% of participants. The overwhelming majority of participants (84%) indicated they would likely review a recording of similar skills programs if these were made available. Most participants (78%) reported that they would prefer mental health skills programs to last between 1 and 2 hours, with the remaining participants preferring programs shorter than 1 hour. Participants were also asked to report a form of treatment they would be most likely to pursue if they were experiencing mental health concerns, and 62% of participants indicated a preference for informal care from family members.
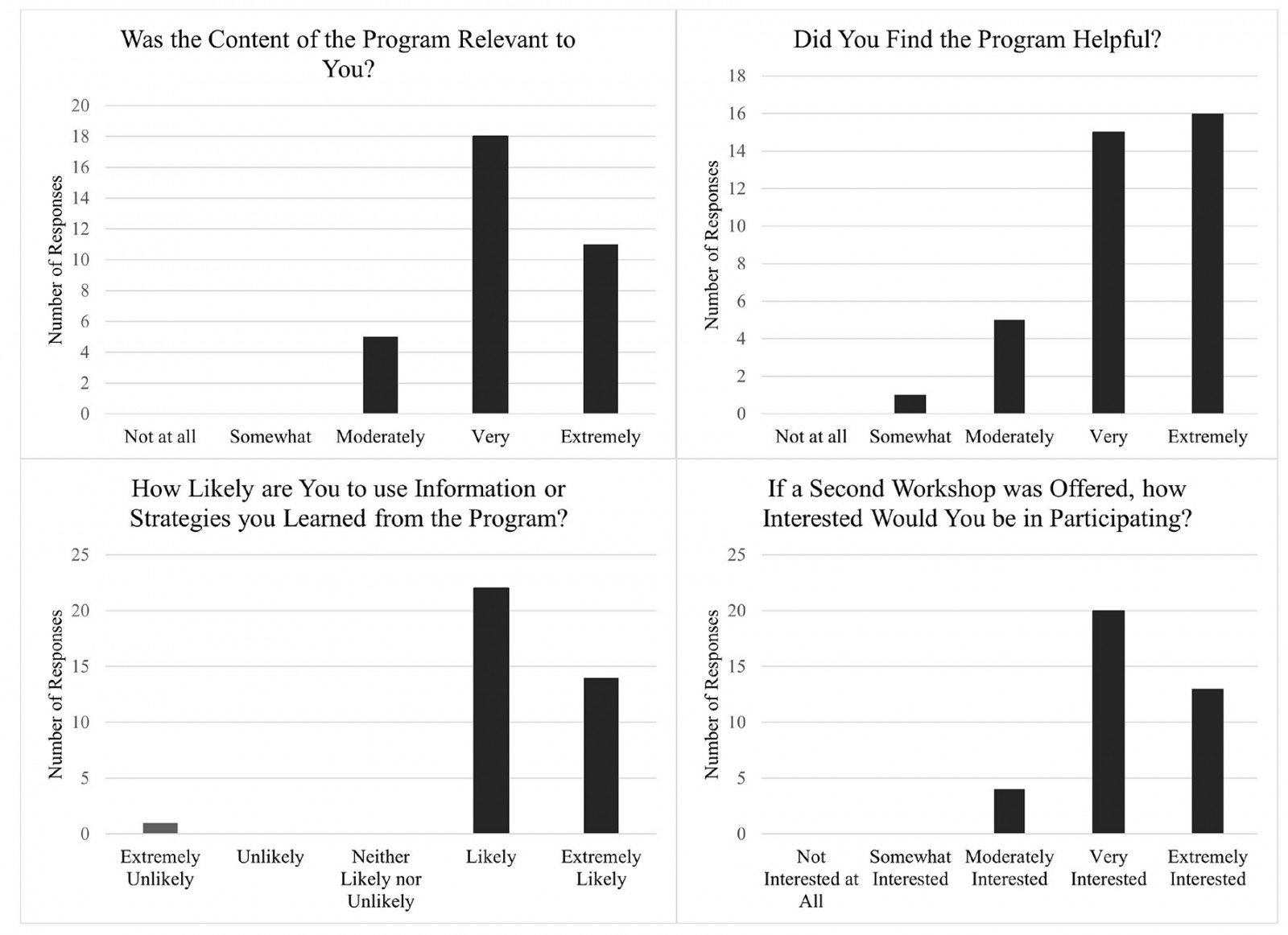 Figure 2: Participant feedback on program (reported post-intervention, N=37).
Figure 2: Participant feedback on program (reported post-intervention, N=37).
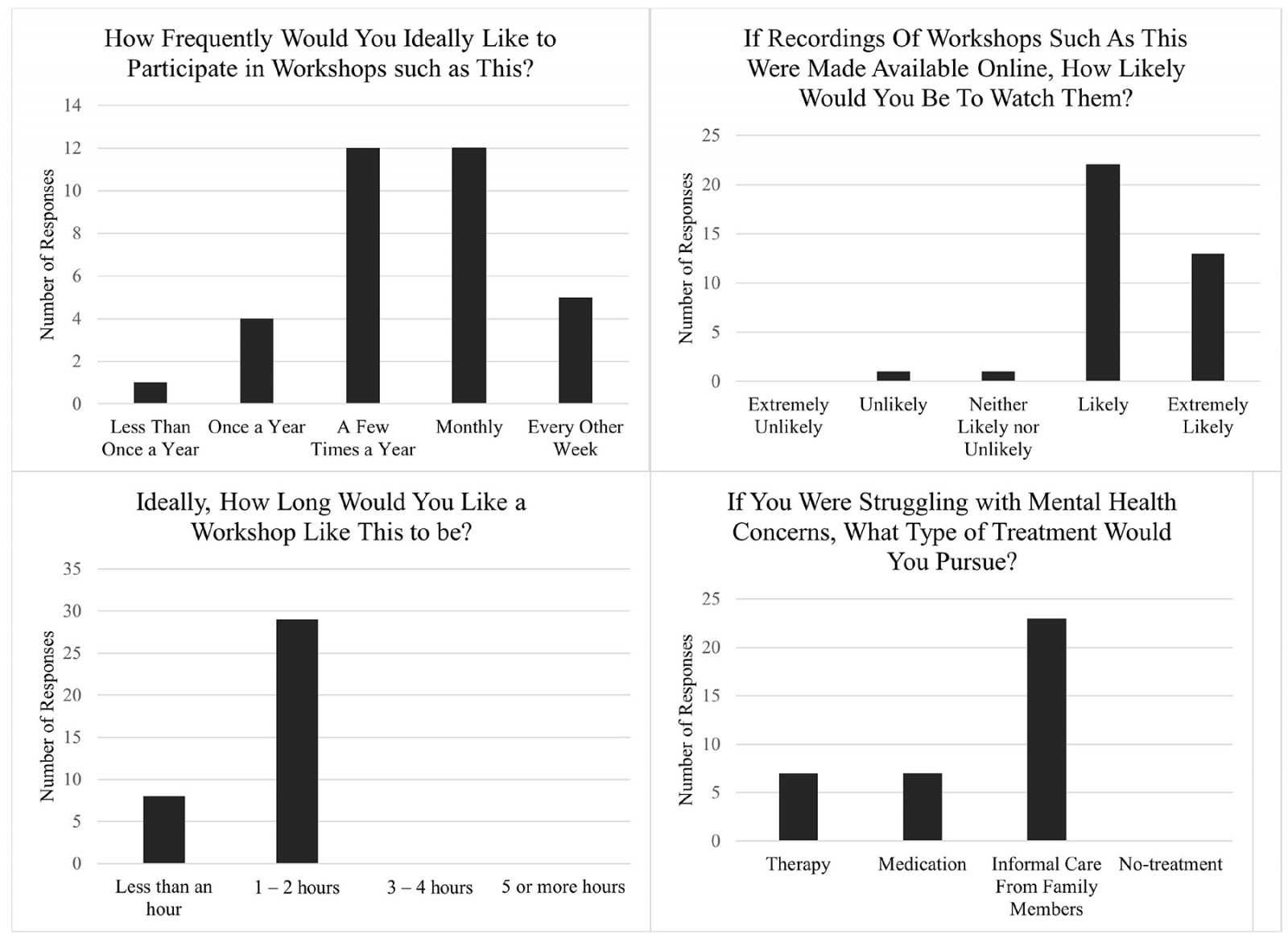 Figure 3: General participant feedback (reported post-intervention, N=37).
Figure 3: General participant feedback (reported post-intervention, N=37).
Change in informal care skills
The program was advertised as offering skills to those who wanted to improve in their ability to help a friend or family member with mental health challenges. All participants reported that they had a friend or family member in mind when signing up for the program. Before the program, immediately following the program, and at a 1-month follow-up, participants reported how much they believed the program would impact their ability to provide support to the person they had in mind. A repeated-measures ANOVA indicated that total scores on the program impact questionnaire differed across the three time points: F(2,36)=4.59, p=0.02. A posthoc comparison using paired sample t-test next compared differences between each time point, and showed a significant though modest increase from pre-intervention (mean=20.05, SD=1.81) to post-intervention (mean=20.97, SD=1.92), t(36)=2.58, p=0.01, d=0.37. Change from pre-intervention to follow-up (mean=21.44, SD=2.34) was also significant, with a similar magnitude of difference, t(35)=2.57, p=0.01, d=0.43. The post-intervention and follow-up scores did not differ significantly (p=0.29).
Participants were also presented with a set of items assessing their confidence in providing support to friends and family members. For support confidence (F(2,36)=11.14, p=0.0002) there was evidence of differences across the three time points. Posthoc t-tests revealed that support confidence significantly increased pre- to post-intervention (pre-intervention: mean=24.14, SD=2.61; post-intervention: mean=25.86, SD=1.89), t(36)=4.15, p=0.0002, d=0.68. From pre-intervention to follow-up (mean=25.89, SD=2.33), support confidence increased, with the size of this effect being medium, t(35)=3.89, p=0.0004, d=0.65. There was no evidence of change in support confidence between post-intervention and follow-up (p=0.96).
Change in hope
Using repeated-measures ANOVA, we evaluated potential change in each of the THS subscales across time. For the agency subscale, there was a significant effect of time (F(2,36)=4.63, p=0.02). Post-hoc t-tests showed no differences from pre-intervention (mean=23.33, SD=4.09) to post-intervention (mean=24.65, SD=3.09, p=0.10). However, change from pre-intervention to follow-up (mean=25.81, SD=2.63) was significant, with a modest magnitude, t(36)=2.89, p=0.007, d=0.48. Although scores improved numerically from post-intervention to follow-up, this difference was not significant (p=0.06).
For the pathway subscale, there was a significant effect of time (F(2,36)=6.21, p=0.005). This appeared to be driven by improvements at the follow-up time point, with differences between pre-intervention (mean=22.16, SD=4.39) and follow-up (mean=24.69, SD=2.91) as well as post-intervention (mean=22.92, SD=3.67) and follow-up being significant (pre-intervention to follow-up: t(35)=3.37, p=0.002, d=0.56; post-intervention to follow-up: t(35)=2.84, p=0.007, d=0.47). The difference between pre-intervention and post-intervention was not significant (p=0.23).
Change in psychological symptoms
Symptoms of depression and anxiety were assessed from prior to the skills program to 1 month following the program. Paired sample t-tests compared change in symptoms pre-intervention to follow-up. For anxiety symptoms, there was a significant medium-sized change from pre-intervention (mean=9.13, SD=4.25) to the 1-month follow-up (mean=7.14, SD=3.20), t(35)=–3.31, p=0.002, d=0.55. For depression symptoms, the observed reduction in symptoms from the pre-intervention (mean=9.97, SD=4.74) to the 1-month follow-up (mean=8.84, SD=4.66) was not significant, t(35)=–1.46, p=0.15, d=0.24. As the initial means reflect, the average depression and anxiety symptoms prior to the program and at follow-up were in the mild range27,28.
Change in CBT skills
CBT skills were self-reported by participants prior to the program and 1 month following the program. Paired sample t-tests pre-intervention to the 1-month follow-up revealed that changes in CBT skills on the four skill subscales were not significant (p>0.17 for all).
Discussion
The first goal of this study was to test the potential benefits of the Friends and Family for Mental Health Program. Our tests of program benefits supported the program as a potential means of improving informal care skills, hope, anxiety, and functional impairment. However, CBT skills did not show significant change. The second goal of this study was to collect feedback to inform program refinement. These surveys indicated that participants found the program helpful and relevant. Participants also expressed considerable interest in additional program offerings and other psychological resources being made available.
To assess informal care skills in this study, we used questionnaires evaluating the program’s impact on the participants’ most important caregiving relationship and the participants’ confidence providing informal care. Observed increases for both sets of items provide evidence suggesting informal care was enhanced. We also observed changes in hope, albeit only at the 1-month follow-up. One possibility is that participants’ later increase in hope is a consequence of changes in attitudes that required greater exposure to the program strategies than the initial program offering of 1 hour and 15 minutes.
Participants did not report increases in CBT skills between the two time points at which CBT skills were assessed: pre-intervention and at a 1-month follow-up. The brief intervention used in this study may not have been an adequate dose of skills training to significantly improve CBT skills. Another possibility is that the measure used in this study, the SERQ, was not adequately suited to assessing the skills used by participants. The SERQ was developed to assess the use of skills to manage individual mental health concerns19. Participants seeking to learn skills to help improve informal caregiving may employ skills in a manner that was not well represented by a measure assessing CBT skills for individual mental health concerns. Participants in this study reported improvements to informal caregiving skills, which could itself be conceptualized as a form of CBT skill gains. The use of other CBT skills measures with item prompts reflecting other-directed coping skill use may be an important area of focus for future research.
As having loved ones with mental health concerns is itself associated with an exacerbation of psychological symptoms, a joint goal of the program is also to reduce existing psychological symptoms and to reduce the risk that the stress of providing informal care could increase participants’ psychological symptoms. We found a medium-sized reduction in anxiety symptoms and a non-significant, small reduction in depression symptoms at the 1-month follow-up. We also asked participants to report the form of treatment they would pursue if they were struggling with mental health concerns and found that most participants (62%) expressed a preference for informal care. Experts in rural mental health have expressed the view that informal caregiving is more common in more rural areas5, but the mental health treatment preferences of those in rural areas has not been carefully characterized empirically. Our study suggests – at least among our participants who signed up to participate in a study involving an intervention fostering informal caregiving skills – a notable preference for informal caregiving in their own care. To what extent informal caregiving is preferred generally, and in rural areas in particular, is an area for future research.
Another goal of this study was to collect participant feedback to inform program development. Results of these surveys indicated that participants found the program helpful, felt the program content was relevant to them, and were interested in further participation in similar programs. Participants had high expectations that the program would be useful, and it was shown that confidence in the benefits of the program when working with friends and family members increased pre- to post-intervention. This high confidence may have been a catalyst for the effects of this program. Indeed, expectation for the benefits of psychological treatment is a reliable prognostic indicator32. We also collected information to inform decisions regarding program length, program frequency, and the provision of program recordings. These indicated participants preferred brief programs lasting between 1 and 2 hours, that participants would prefer to attend such programs multiple times a year, and that participants would be interested in reviewing recordings. Another area of focus could be to further encourage participants to practice and make use of CBT skills both during and after the program. Though this was a major feature of the program in its current iteration, our finding that CBT skills did not significantly improve may be an indication that a further emphasis on practicing CBT skills could add to the benefit of these groups.
The intervention was provided online in an effort to reduce barriers that could interfere with participants easily accessing it. However, it is important to note that internet connectivity differs considerably across the US and is especially limited in some remote rural areas33. As internet access increases, providers will need to continue to evaluate the pros and cons of online versus in-person offerings. Though online interventions allow for such trainings to reach a large area at a low cost, it may not be feasible for some rural residents to effectively participate in such program offerings. Providing interventions both online and in person may provide the greatest opportunity for potentially interested rural residents to participate in mental health skills trainings.
This study has several important limitations. The small sample size used in this pilot study limited our power and may have prevented us from detecting effects of interest. Our sample was overwhelmingly male and largely college educated. We suspect that the intervention appealed more to men and those with greater educational attainment. One contributing factor may be that frequent online newspaper readers are more often men34. It is also noteworthy that previous research on online group interventions indicates that men participate in higher frequency than women35,36. The anonymity that an online program affords may appeal to men in particular36. Given that men utilize psychotherapy less frequently than women37, such programs may be a particularly useful means of reaching them. Research on online newspaper readers also indicates that regular online newspaper readers tend to be more educated than non-readers34, which may have also influenced the study sample. It could also be that those who pursued more education are also more interested in educational webinars. Future research should consider various methods of study recruitment so that methods of reaching the full range of those who may benefit from intervention offerings can be better understood. Gauging the appeal of such a program to women and less educated adults is an important goal for future research. Regardless, the sample composition limits the generalizability of the study’s findings. Additionally, though participants self-identified as an informal caregiver for a friend or family member, we otherwise lacked information about the nature of participants’ informal caregiving relationships. In future research, it would be useful to characterize these informal caregiving relationships and consider if the impact of informal caregiving skills programs differs across different kinds of informal care relationships. Similarly, our lack of an experimental comparison condition prevents us from determining with certainty whether the changes we observed were due to the intervention. Though our findings are promising, only evidence coming from a randomized comparison can allow accurate determination of intervention benefits. The benefits of such interventions remains a sizable gap in the treatment literature, and we encourage further research of this type.
Conclusion
This study provided preliminary support for the Friends and Family for Mental Health Program. Addressing the unmet mental health needs in rural areas is a complex issue. It is an issue that calls for multifaceted solutions, involving greater availability of existing treatments and novel solutions that can add to the efficacy and reach of psychological interventions in rural areas5. One potential means of addressing some of this unmet need is to draw on and enhance the informal care that is already common to rural areas. With this program, we sought to build on this resource. Findings indicated the program improved informal care skills, anxiety symptoms, and hope. This preliminary evidence suggests mental health programs focused on skills relevant to informal caregiving may be beneficial in rural areas. Considering that such programs are low in risk and cost, we encourage the further provision of such programs in rural areas.
Funding
This research was supported by a Psi-Chi Mamie Phipps Clark Diversity Research Grant and by an Ohio State University Alumni Grant for Graduate Research and Scholarship, both awarded to the first author.
Conflicts of interest
The authors declare that they have no conflict of interest.
References
You might also be interested in:
2020 - A mandatory bonding service program and its effects on the perspectives of young doctors in Nepal
2016 - The Cumbria Rural Health Forum: initiating change and moving forward with technology
2007 - Breast, colon, and prostate screening in the adult population of Croatia: does rural origin matter?

