Introduction
Primary care is considered to be an essential component of health care for addressing community health problems1. Primary care physicians, also referred to as GPs or family doctors, are widely considered the foundation of successful healthcare systems and, as such, their training is pivotal in ensuring comprehensive care2. Advanced Skills Training (AST) is an opportunity for GPs to further refine their skills across one or more narrower medical specialties that require larger populations and/or more advanced technology than smaller communities can support. Training in a wide range of advanced skills is possible, including procedural (eg anaesthetics, emergency medicine and obstetrics) or non-procedural skills (eg in mental health, Aboriginal and Torres Strait Islander Peoples’ health, internal medicine)3,4. These extend the scope of safe practice accessible to local communities5, but training pathways vary considerably between states and regions3. AST among GPs has been found to be beneficial in various ways. Doctors who have completed GP AST report positive experiences and recommend strategies to improve support, including provision of training and career advice, introduction of rural attachments and case studies, development of mentor and peer networks, and advocacy for recognition of advanced rural skills training6.
While the specific components of AST programs may differ across the world, the goal of reducing rural health disparities remains consistent2,3. Over the years, rural training pathways have evolved to suit the needs of rural communities, trainees, trainers, health services and medical colleges7. However, some researchers have argued that current rural training opportunities are missing the mark on bridging the gap between urban and rural health, and rural communities have been used as rotational outposts from urban centres8. Furthermore, the demands on GPs have expanded beyond traditional boundaries, necessitating a re-evaluation of the skills and competencies required to address the complex and multifaceted health needs of diverse patient populations.
Consequently, it is necessary to review the current value and fitness for purpose of AST and ensure that it is promoting a better distributed rural medical workforce to meet the growing demand for coordinated care in rural communities9. Therefore, this review aimed to address the following questions:
- What is the effectiveness of AST programs in improving GPs’ knowledge, attitudes and competence regarding rural clinical practice?
- How do stakeholders – including trainees, patients, management and the community – perceive the impact (value and fitness for purpose) of the AST program in rural clinical practice?
- To what extent are AST programs aligned with the needs of the community served?
Methods
This review was undertaken in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement10 (Supplementary table I). This review was not prospectively registered.
Search strategy
Electronic databases (Medline Ovid, CINAHL, Emcare, Scopus, Web of Science and Informit) were systematically searched for peer-reviewed articles meeting the inclusion criteria in December 2024. The search utilised MeSH subject headings, subject heading terms, phrase searching and truncation. The Polyglot Search Translator from the Systematic Review Accelerator software package developed by Bond University (https://bond.edu.au/iebh/systematic-review-accelerator-sra) was employed to align the search terms for each database11. In addition, a hand search of the reference lists of the included articles was conducted to identify more relevant studies. The search was replicated across three authors (HM, FAA, AS) to ensure consistency. The search terms are provided in Supplementary table 2. The deduplication online software within the Systematic Review Accelerator package was used to remove duplicate articles12.
Inclusion and exclusion criteria
The review's inclusion criteria encompassed (1) peer-reviewed articles in English, (2) studies conducted between 2000 and 2024, (3) studies pertaining to general practice (or equivalent such as family practice or family medicine) and (4) studies addressing at least one of the three research questions. Studies not meeting these criteria or classified as literature reviews or commentaries were excluded. The inclusion period was selected to represent contemporary and relevant evidence, as medicine is a dynamic field and has changed considerably since the turn of the century13,14. The selection process is illustrated in Figure 1. The inclusion and exclusion process was managed using the web-based app Rayyan (Rayyan; https://www.rayyan.ai)15.
There are various definitions of AST across the globe. For the purpose of this review, the authors defined AST as an accredited training program for GPs designed to enhance skills in a specific procedural or non-procedural training area. AST requires either a focused residency-based track, integrated education rotation or fellowship program that lasts at least 6 months.
Data extraction and synthesis
Three authors (HM, AS and FAA) conducted initial screening of article titles and abstracts, with additional support and frequent discussions with authors FOA, BM-A and EA. Articles that did not meet the inclusion criteria were excluded, while potentially eligible articles underwent a full-text screening process. Any disagreements were resolved through weekly consensus meetings. An Excel data extraction form was created to extract pertinent information from all included studies. Descriptive data such as author details, publication year, study aims, study period, AST definition, perspectives, participants and key findings were extracted from the articles meeting inclusion criteria. Each article was analysed for statements and concepts relevant to the research question and study objectives.
Risk of bias assessment
Due to the diverse nature of the studies included in the review the Quality Assessment for Diverse Studies (QuADS) tool was used16. This tool is specifically designed to ascertain the methodological robustness, reporting quality and overall transparency of mixed-methods studies. The QuADS tool has 13 items rated on a four-point scale (0–3), yielding a maximum possible score of 39 points. The evaluated criteria encompass various aspects, including (1) ‘theoretical or conceptual underpinning to the research’, (2) ‘statement of research aim(s)’, (3) ‘clear description of research setting and target population’, (4) ‘appropriateness of study design to address research aim(s)’, (5) ‘appropriate sampling to address the research aims’, (6) ‘rationale for choice of data collection tools’, (7) appropriateness of the format and content of data collection tools’, (8) description of data collection procedures, (9) ‘recruitment data provided’, (10) justification for analytic methods’, (11) ‘appropriateness of analytic methods to answer research aims’, (12) ‘evidence of stakeholders involvement’, and (13) ‘critical discussion of strengths and limitations’. Two independent reviewers (AS and HM) appraised the included papers. The range of cumulative scores for the included studies was 15–34 points, with a median score of 26 points. Lower scores were noted in criteria such as sampling appropriateness, recruitment data, stakeholder involvement, critical discussion of strengths and limitations, and rationale for data collection tool selection. This assessment highlights reporting limitations rather than making a qualitative judgement about the studies. As a result, none of the studies were excluded based on this evaluation17. The results of the risk of bias assessment are provided in Supplementary table 3.
Results
The search results yielded 18,795 articles, of which 8911 were screened after the removal of duplicate entries. Of the 8911 titles and abstracts screened, 47 were assessed for full-text eligibility and 16 were included in the systematic review. Three articles could not be retrieved18-20. This process is illustrated in the PRISMA flow diagram (Fig1).
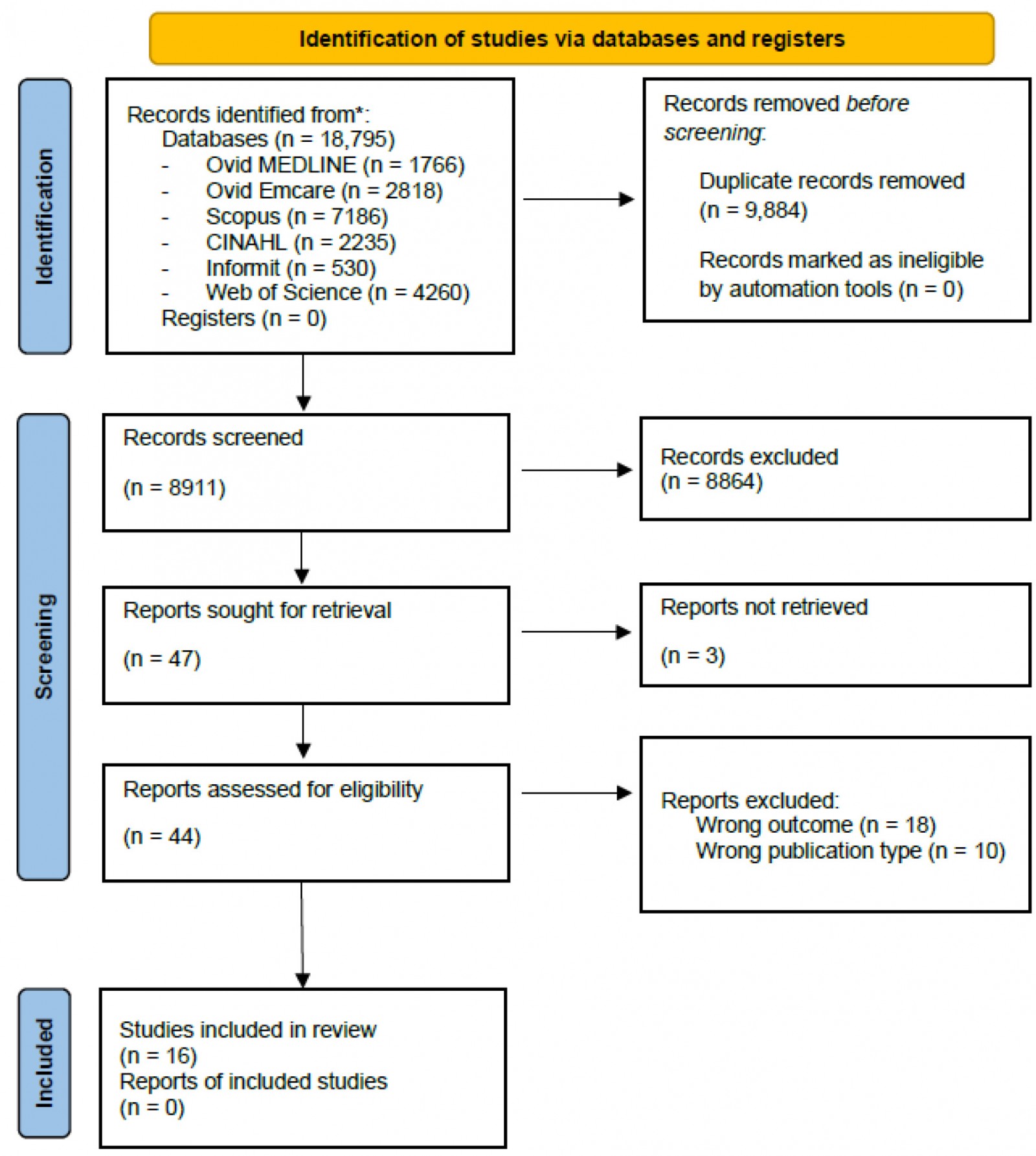 Figure 1: PRISMA flow diagram for Advanced Skills Training systematic review10
Figure 1: PRISMA flow diagram for Advanced Skills Training systematic review10
Characteristics of studies
Of the 16 included studies, 11 employed qualitative study designs (n=11; 68.8%), while five adopted quantitative study designs (n=5, 31.3 %; Table 1). The studies were conducted in Canada (n=5, 31.3%), Australia (n=5, 31.3%), the US (n=4, 25.0%) and England (n=2, 12.5%) (Table 1).
Table 1: Advanced Skills Training systematic review – characteristics of included studies
| Author (year) | Setting | Aim | Participants | AST Definition/description | Key findings |
|---|---|---|---|---|---|
| Allan (2011)21 | New South Wales, Australia (2011) | To describe the establishment and operations of an Advanced Rural Skills Training program at the Lyndon Community – a rural drug and alcohol treatment organisation. | GP registrars (n=5) | General Practitioner Advanced Rural Skills Training program funded by New South Wales Health | Registrars participating in the addiction medicine rotation program positively impacted and improved their prospective professional practice. |
| Butler et al (2013)22 | Milwaukee, Wisconsin, US | To describe the development of a Behavioural Medicine track in a family medicine residency to train physicians to apply advanced skills in psychosocial medicine, psychiatric care and behavioural medicine. | Residents (n=4) | Residency-based Behavioural Medicine track offered at Columbia-St. Mary's Family Medicine Program | The Behavioural Medicine track attracted medical students to the residency program. Feedback from graduates suggests successful incorporation of behavioural medicine skills and abilities in clinical practice, regular use of counselling techniques and a confidence in treating common psychiatric disorders. |
| Cope and Alberti (2020)23 | North East England | To improve understanding of integrative training posts in general practice, to determine why trainees choose to undertake this experience and to explore the impact of that decision on personal and professional development. | GP trainees (focus groups n=11; one-on-one interviews n=4) | Education integrated training posts – 6-month rotation where half the work week is spent in primary care and the other half in a specialty | The overarching theme emerging from the participants’ views of their experiences was identity formation. Trainees reflected on their personal identity, professional identity and identity associated with the community. |
| Correia et al (2022)†24 | Canada | To examine how the care of the elderly CAC impacts primary care for older patients and to explore factors that impact group practice. | Family physicians (n=39); resident trainees (n=6); administrative staff (n=2); geriatrician (n=1) | CAC offered by the College of Family Physicians of Canada | Training enabled family physicians to deliver geriatric-focused care, improving access, continuity and comprehensive services for older patients, especially in under-resourced areas. While the CAC enhanced physician competence and career opportunities, challenges such as limited financial incentives, high training costs and inconsistent remuneration models were noted. |
| Dale et al (2017)25 | West Midlands, England (2014) |
To investigate the experience of GPs undertaking a fellowship program designed to provide advanced skills training in urgent care, integrated care, leadership and academic practice and its impact on subsequent career development. |
GP Fellows (n=7) | 1-year fellowship program providing AST in urgent care, integrated care, leadership and academic practice | The fellowship was perceived as well rounded in providing opportunities for skill development, academic progression and confidence-building. Graduates reported improved employability, holding diverse primary care/urgency care clinical and leadership roles. |
| Eden and Peterson (2018)26 | US | To understand the challenges faced by family practitioners when acquiring skills and providing advanced maternity care. | Stakeholders in family medicine maternity care (fellowship directors n=21, past fellows n=19, residency directors n=10) | Maternity care/obstetric fellowships recognised by the American Academy of Family Physicians and the American Board of Physician Specialists | Three primary challenges were recognised for family physicians obtaining maternity care skills including sufficient training, credentialling (ie privileges to perform caesarean sections highly variable and unpredictable) and interprofessional conflicts or ‘turf wars’. |
| Elma et al (2023)27 | Canada (November 2019 – January 2020) | To investigate perceptions of the CAC program from both CAC holders and family physicians without the CAC. | Family physicians (n=1525) | CAC offered by the College of Family Physicians of Canada | Physicians reported that CACs promoted collaboration, benefited their professional practice and benefited their communities by reducing barriers to accessing health care. A reported unintended consequence was the devaluation of expertise for family physicians who do not hold CACs. |
| Grierson et al (2021) †28 | Canada (September 2018 – June 2019) | To assess the impact of the CAC in care of the elderly, family practice anaesthesia, palliative care, and sports and exercise medicine. | Family physicians (n=39), resident trainees (n=6), administrative staff (n=2), geriatrician (n=1) | CAC offered by the College of Family Physicians of Canada | A mixture of positive and negative impacts of extended skills through CACs was identified. Positive impacts included expanded scope of services, reduced patient travel and improved continuity of care. Negative impacts reported were promotion of personal clinical interests above community need, administrative barriers and limited collaboration due to remuneration structures. |
| Howard et al (2023)†29 | Canada (September 2018 – June 2019) | To explore the ways that family physicians with enhanced palliative care skills work in their communities, the factors that influence their practice and the perceived impacts. | Family physicians (n=21) | Palliative care CAC offered by the College of Family Physicians of Canada | Palliative care physicians used mixed or focused practice models, offering care through collaboration with other physicians or taking over as the main provider. The integration of palliative care expertise was influenced by payment structures, referral systems and interprofessional willingness to consult. |
| Kitchener (2020)30 | Queensland, Australia (2002, 2015) | To assess the medical workforce return on regional investment in training by local stakeholders in terms of qualified GPs remaining in the region. | GP registrars (n=222) | Australian General Practice Training registrars with Advanced Rural Skills Training | The completion of Advanced Rural Skills Training by Australian graduates and trainees led to enhanced retention and local return on training investment. |
| Magee et al (2015)31 | Rhode Island, US (1991, 2011) | To describe the maternal–child health fellowship of the Brown University Department of Family Medicine, located in an urban, underserved setting, and the careers of its graduates. | Family physicians (n=17) | Maternal–child health fellowship | Most fellowship graduates use their advanced skills and provide maternity care (with half serving as primary surgeons in caesarean sections, mainly in community hospitals). Almost all alumni hold academic positions and actively contribute to teaching in their family medicine departments. |
| McGrail and O’Sullivan (2020)32 | Australia (2008, 2013 and 2017) | To evaluate the benefit of rural faculties for supporting a geographically distributed rural GP workforce and at a broader scope. | Clinically active GPs (2008 n=3930, 2013 n=2936, 2017 n=3185) | Specialised training of at least 6 months, which is outside the normal scope of practice for GPs | In comparison to those without such qualifications, those with their FARGP (29–34%) or FACRRM (26–31%) were more likely to use their advanced skills. Those who graduated after 1995 were more likely to maintain their advanced skills if they were FACRRM graduates in comparison to FARGP graduates. |
| McKenzie et al (2013)33 | Queensland, Australia |
(1) Describe where GPs practise in the 5 years after advanced rural skills training, (2) describe the proportion of doctors using their advanced skills, (3) measure doctors’ ratings of the quality of support and how critical the year directly following training is in future career choices and (4) measure the association between support and use of advanced skills. |
Doctors who completed Advanced Rural Skills Training in Queensland between 1995 and 2009 (n=61) | Advanced Rural Skills Training by RACGP and ACCRM | Most respondents (63.9%) were actively applying AST skills when surveyed. Within the initial 5 years post-training, the utilisation of advanced skills declined from 75.4% to 61.1%. The quality of support received during that period varied, with 21.4% rating it as ‘very poor’. There was a significant association between the support received in the year following training and the subsequent use of skills 3 years later. |
| McKenzie et al (2013)6 | Queensland, Australia | To investigate experiences of support during GP Advanced Rural Skills Training and identify strategies to improve support. | Doctors who completed Advanced Rural Skills Training in Queensland between 1995 and 2009 (n=61) | Advanced Rural Skills Training | The findings were translated into a support framework with three thematic areas, encompassing strategies such as offering training and career advice for immediate application of advanced skills, integrating rural elements into training, establishing GP mentor and peer networks for comprehensive support and advocating for better recognition of Advanced Rural Skills Training. |
| Romain et al (2015)34 | Oregon and Michigan, US (2014) | To describe two family medicine residency curricular experiences designed to allow GPs to care for patients with severe and persistent mental illness. | Residents (number not clear) | Family medicine residency programs for residents develop advanced skills (caring for patients with adverse mental health outcomes) | All participants found the program beneficial for their current or future practice and gave positive evaluations, citing advantages such as working with underserved populations, increased awareness of healthcare costs, enhanced skills in psychiatric and low health literacy patient care, interdisciplinary teamwork and positive feedback from group home leaders. |
| Thornton et al (2022) †35 | Canada | To explore the impact of the sport and exercise medicine CAC on the delivery of comprehensive care across Canada | Family physicians (n=39), resident trainees (n=6), administrative staff (n=2), geriatrician (n=1) | CAC in sport and exercise medicine offered by the College of Family Physicians of Canada | Participants reported the sport and exercise medicine CAC enhanced wellbeing, job satisfaction, collaboration with other healthcare providers and comprehensive care. Challenges regarding renumeration and community alignment were identified, specifically where practitioners prioritised niche interests over broader community needs. |
† This study used the same qualitative dataset as a broader project.
CAC, Certificate of Added Competence. FACRRM, Fellowship of the Australian College of Rural and Remote Medicine. FARGP, Fellowship in Advanced Rural General Practice. RACGP, Royal Australian College of General Practitioners.
Definitions of advanced training
The definition and scope of AST programs varied across the literature. In Canada, the College of Family Physicians of Canada’s Certificate of Added Competence (CAC) was explored by Correia et al24, Elma et al27, Grierson et al28, Howard et al29 and Thornton et al35. This program requires successful completion of an accredited 1-year enhanced skills residency program or through a practice-eligibility route29. In Australia, two studies by McKenzie et al6,33, one by Kitchener30 and one by McGrail and O’Sullivan32 reported on the Advanced Rural Skills Training programs under the Royal Australian College of General Practitioners and the Australian College of Rural and Remote Medicine, which involve 12 months full-time-equivalent in an accredited training post. In England, integrated training posts were utilised to develop educational advanced skills in a study by Cope and Alberti, which were described as 6-month rotations where half of the work week is spent in primary care and the other half in a specialty23.
Other studies defined the training as ‘tracks’, extended fellowships, residency programs or placements. In England, Dale et al investigated a 1-year fellowship that aimed to provide advanced skills in urgent care, integrated care, leadership and academic practice25. At Brown University in the US, Magee et al explored the outcomes of a maternal–child health fellowship, which involved a 1- or 2-year program with integrated training at local federally qualified community health centres and a private multi-specialty group31. Regarding mental health ASTs, Allen et al 21 described a program with a non-governmental drug and alcohol agency, the Lyndon Community, which falls under the behavioural medicine strand of the New South Wales Health funded General Practitioner Advanced Rural Skills Training Program. At the Columbia-St. Mary’s Family Medicine program in the US, Butler et al22 described a Behavioural Medicine track developed for residents to obtain advanced skills in psychosocial and behavioural medicine and psychiatric care. Romain et al explored two family medicine residency programs designed to develop advanced skills in behavioural medicine for patients with severe and persistent mental illness34.
Improvements to clinical practice
Across the literature, participants noted improvements in their knowledge, attitudes and competence regarding their clinical practice. For example, Allan described the impact of an AST program at a rural drug and alcohol treatment centre, and reported that registrars indicated the experience influenced and enhanced their practice21. The opportunity allowed residents to practise psychosocial interventions (eg motivational interviewing), conducting a research project and understanding the relationship between substance misuse and mental health21. In England, trainees who undertook the 1-year fellowship program also positively rated their experiences and felt that their clinical work contributed to their ability to manage subacute and acute cases in the community25. This was echoed in the feedback provided by family physicians who undertook residency programs in the US to prepare for the care of patients with severe and persistent mental illness, in which all participants responded that the program was useful for their current or future practice34. Similarly, family physicians in Canada with advanced skills in palliative care and care of the elderly reported enhanced clinical competence to manage complex issues24,29. Students in Rhode Island in the US also remarked on their use of clinical skills in the community, where 92% of graduates of a maternal–child health fellowship were able to obtain maternity care privileges post-fellowship and currently manage high-risk medical conditions (eg pre-eclampsia, gestational diabetes)31. After an educational training post through Health Education England North East, participants saw improvement in their consultation skills23. They noted that their ability to use their experience teaching medical students was transferrable to their clinical practice, where they were able to apply similar teaching and phrases23. On the other hand, in Canada, Elma et al reported that only 22% of CAC holders indicated that the training provided less clinical uncertainty27.
Value and fitness for purpose
One of the ways in which the value of AST programs is exemplified is the continued use of skills following the training. For example, in Queensland, Australia, where GPs with a range of advanced skills were surveyed in 2013, the majority of respondents reported actively using the skills related to their AST (63.9%)33. The use of skills following the AST was associated with support in the first year after training, and those who reported good to very good support were more likely to use their advanced skills33. In another Australian study, the faculties in which training was undertaken impacted skill maintenance, with Fellowship of the Australian College of Rural and Remote Medicine graduates more likely to use their skill in their job than Fellowship in Advanced Rural General Practice graduates32. Skill utility was also exhibited on a smaller scale in the US, where one of the graduates from the Columbia-St. Mary’s Behavioural Medicine track reported actively using the mindfulness techniques acquired during training in most clinical encounters22. Barriers to skill utility were noted across Canadian studies, including workload balance and remuneration24,28,29,35.
Trainees also valued the additional skills developed beyond clinical practice, including community engagement opportunities provided by the AST experience. For example, trainees in the West Midlands, England, viewed their ability to apply their knowledge about community resources, connect with other professionals in the community and seek advice from those professionals as highly beneficial25. The trainees also reported that the program opened future work opportunities, and that they felt their acquired skills were highly valued by future employers25. Additionally, in Canada, physicians with advanced skills in palliative care and care of the elderly noted the value of their credentials in providing education to their generalist colleagues and for pursuing academic and leadership roles24,29. In another example, across two residency programs in Oregon and Michigan in the US, trainees acquiring advanced skills in caring for patients with severe and persistent mental illness cited many benefits including greater awareness of patient healthcare costs, improved comfortability with care for patients with psychiatric illness, better care for patients with low health literacy, and improved management of psychiatric illness and chronic disease, work with an interdisciplinary team and work in a community health centre context34. Similarly, trainees in North East England reported that their time spent in the primary care setting was useful for professional development; improved their confidence, time management and organisation; and broadened their perspectives23.
Another way in which the value of AST programs was exemplified was in rural workforce retention, and findings from an Australian study indicated that graduates who had completed AST improved local return on investment in terms of qualified GPs remaining in the area30. More specifically, those who completed an advanced skill were almost three times more likely to remain in rural practice than those who did not (odds ratio 2.8; 95% confidence interval 1.6–5.1)30. AST programs also impacted earning potential, with the majority (60.0%) of trainees in Rhode Island, US, stating that they believed their maternal–child health fellowship led them to earn similar or higher salaries than their colleagues who did not complete the program31. However, in a Canadian study, only 17.8% of CAC holders reported higher remuneration as a result of their advanced skills, underscoring the challenges in aligning financial compensation with the added responsibilities and expertise of advanced training27.
Some challenges were reported for those undertaking AST programs. Some examples include barriers to inclusion on remote visits21, time efficiency and time management21,23, issues with workload fluctuation23,26, support in career decisions and use of advanced skills6, gaps between training and use of skills6, peer acknowledgement6,24,26 and difficulties obtaining learning opportunities when preference was given to registrars of other specialist colleges6,26. Another challenge was the differences between the hospital settings in which training occurred and the rural contexts in which the skills would be applied6.
Regarding unintended consequences of advanced training, in Canada, physicians without advanced skills strongly agreed that the CAC devalued the expertise of those who did not hold one and were concerned that the certification would inflate the minimum credentials required to practise27. Further, concerns regarding physicians with advanced skills shifting away from generalist care in favour of specialist services were highlighted by researchers in Canada24,28. For example, Thornton et al35 described concerns around sport and exercise medicine CAC holders who choose to see athletes exclusively.
To improve the fitness for purpose of AST programs, participants in Queensland recommended that personal objectives should be matched to training requirements (on-call requirements, maintenance of credentials, increased responsibility)6. Forward planning was also recommended by participants, to encourage appropriate selection of training post to develop learning objectives and build professional networks6. In a qualitative analysis regarding advanced maternity skills in the US, researchers recommended enhancing training in advanced maternity care by involving obstetricians to fill training gaps, moving toward competency-based credentialling and improving team-based care to facilitate interprofessional collaboration26. In Canada, policies encouraging part-time enhanced-skill roles were suggested to ensure physicians continue to contribute to generalist care while utilising their advanced training28.
Responding to community needs
The impact of advanced training on health demand was discussed by trainees interviewed in England25, Australia21 and the US22. For example, in Australia, feedback received about a drug and alcohol AST program indicated that the program reduced the demand on local GPs21. In another example, a graduate of the Columbia-St. Mary’s Behavioural Medicine track negotiated a 40-minute counselling appointment with their employer22. The trainee noted that this appointment is routinely filled, signifying her capacity to help meet the community’s need for mental health services22. In England, trainees provided examples of how the program was able to help them facilitate community-based specialist services for patients more efficiently to avoid emergency department presentations and unplanned admissions25. Canadian physicians noted improvements in access to health care due to CACs, particularly for those who reside in rural and remote areas and would otherwise need to travel to a specialist outside of the community27,28. Participants also cited concerns about physicians selecting extended skills based on personal and professional interests above community needs28,35.
Discussion
Advanced skills training is an important component of building a rural healthcare workforce. This systematic review synthesised evidence from 16 studies that together highlighted improvements to clinical practice, the value and fitness for purpose of AST programs, and alignment with community needs.
The exploration of various studies highlights the heterogeneity in defining and implementing AST programs among GPs. These programs range from year-long fellowships and integrated training posts in England to tracks, residency programs and placements in the US, to certificates in Canada and fellowships in Australia. Notably, the diversity in program structures raises questions about standardisation, necessitating a deeper understanding of the specific components that contribute to the effectiveness of these training initiatives. This variability underscores the need for standardisation to facilitate effective communication, comparison and evaluation of AST programs worldwide.
Across the literature, participants in AST programs reported enhancements in their knowledge, attitudes and competence related to clinical practice. From psychosocial interventions and research projects to managing subacute and acute cases in the community, the positive impact resonated across different contexts. Nonetheless, evidence suggests that substantial disparities in health care persist for individuals residing in rural and remote areas36. Patients in these communities are more likely to experience adverse health outcomes compared to those in urban areas37. Notably, the feedback from participants who prepared for the care of patients with severe and persistent mental illness in the US and England emphasises the practical relevance and immediate applicability of the acquired skills, reinforcing the value of AST in shaping competent and versatile practitioners25,34. The positive impressions demonstrated by the participants in the various studies underscore the need to expand AST to other regions and countries to ensure adequate and quality delivery of essential health services to people in rural and remote areas to improve health outcomes. That said, context-specific considerations are essential, as some GPs may not return to general practice after completing their AST.
In relation to perceptions of the value and fitness for purpose of AST in rural clinical practice, participants reported that they actively used the advanced skills they had acquired in their clinical practice after completing AST in Australia and the US22,33, indicating practical application of the skills obtained. This also confirmed that the value of AST programs extends beyond the training period. The correlation between post-training support and the ongoing use of acquired skills highlights the importance of sustained mentorship and professional assistance. Soft skills development and community engagement opportunities were also highly valued, contributing to a holistic approach to healthcare practice. Moreover, the positive impact on rural workforce retention, as demonstrated in the Australian and US studies, serves as a compelling testament to the long-term benefits of AST on the distribution of skilled healthcare professionals. In addition, evidence suggests that about 7 out of 10 graduates from the Queensland Rural Generalist pathway are still using their AST38. However, the review did not uncover evidence regarding rural retention in Canada or England. While several studies reflected trainee perspectives on the value and fitness for purpose of AST, voices of other stakeholders such as patients, management and the community were rarely amplified in the research. To enable a more holistic view of the impact, value and fitness for purpose of AST programs, future research must be undertaken to capture these perspectives.
There was minimal evidence across the literature that directly addressed AST alignment with community need; nonetheless, some studies indicated positive impacts to health service demand21,22,25. However, Canadian research raised concerns that physicians may select extended skills based on personal and professional interests, which could lead to a mismatch with community needs28,35. The literature did not indicate any formal processes for advanced skill specialty selection to bridge this gap. General practice is considered the backbone of primary health care and is integral to healthy communities39, and therefore it is necessary to ensure that current AST programs are meeting community needs and health priorities. Future research could explore community perspectives to ensure that AST programs are tailored to address the unique needs and challenges of the communities they serve. While the benefits of AST programs are evident, challenges such as barriers to remote visits, time management issues and difficulties in obtaining learning opportunities persist. The importance of addressing these challenges is crucial for optimising the fit-for-purpose nature of AST programs. Recommendations from participants, such as aligning personal objectives with training requirements and forward planning, offer valuable insights for program developers and policymakers aiming to enhance the effectiveness and relevance of AST initiatives.
Strengths and limitations
To the best of our knowledge this is the first systematic review to explore the utility of AST for GPs globally. AST is evolving with integration of technology, interdisciplinary training and public health needs. While a range of advanced skills were explored in the literature, it is noted that some procedural and non-procedural advanced skills may not have been covered, impacting the generalisability of this review. The studies included in the review reflected AST in high-income, English-speaking countries, likely as a result of excluding studies that were not published in the English language. Therefore, other important studies published in different languages and contexts might have been missed.
Conclusion
This systematic review of literature on the utility of AST among GPs revealed a multifaceted perspective with diverse definitions, program structures and outcomes. The likely positive impacts on clinical practice services, continued use of advanced skills, rural workforce retention, alignment with community needs and healthcare outcomes require confirmation through research to demonstrate the value of AST programs. However, the identified challenges necessitate a concerted effort to refine, tailor and coordinate these programs to better suit the evolving needs of both the workforce and the communities they serve. A collaborative approach involving educators, policymakers and practitioners is imperative to shape AST initiatives that are not only comprehensive but also adaptable to the dynamic prospect of primary care.
Acknowledgements
We are grateful to the Australian College of Rural & Remote Medicine for funding this project.
Funding
This study was funded by the Australian College of Rural and Remote Medicine.
Conflicts of interest
The authors declare no conflicts of interest.
References
You might also be interested in:
2022 - Telehealth use in rural and remote health practitioner education: an integrative review
2016 - Doctors as street-level bureaucrats in a rural hospital in South Africa










