Introduction
In Latin America, Indigenous Peoples are among the social groups with the least access to basic health and education services, which makes their ethnic–racial condition a cause of health inequity. Research conducted in some Indigenous communities on these barriers indicates that most of them are cultural in nature1. Some studies have identified risk factors associated with high suicide rates within Indigenous communities. These include economic difficulties, dependence on the state, an inadequate educational system, identity problems, and challenges in the parenting process. Additionally, chronic pain, substance abuse disorders, domestic violence, and the struggle with identity in adolescents transitioning from a tribal identity to a globalized society can lead to feelings of sadness, anguish, and hopelessness2,3.
Systematic reviews have revealed a high prevalence of suicide among Indigenous Peoples, which is connected to social and economic exclusion. This often results in poor health outcomes for these populations. However, community-based programs are frequently not evaluated or have subpar study designs, the interventions are misaligned with Indigenous cultural paradigms, and research on interventions with Indigenous communities is infrequent4-7. In the same way, mental health and wellbeing measurements for Indigenous Peoples are rare, having mostly been developed in Oceania and North America, and often these tools are based on Western concepts or generalized from general population validations. This means that Indigenous Peoples frequently are evaluated with non-Indigenous parameters8. This can also result in inaccurate assessments and misdiagnosis of mental health conditions, as well as a failure to recognize the strengths that Indigenous Peoples may possess in coping with challenges.
In Colombia, the ENSM-2015 (National Mental Health Survey) reported that 8.3% of the adult population identified as Indigenous by self-recognition, and that this group had high poverty rates (26.6%) and exposure to violence associated with displacement (17.8%), higher rates than in other population groups. The prevalence of problems was 8.1%. Of this prevalence, 16.2% was due to excessive alcohol consumption and 7.6% was due to anxiety and depression1. During 2009, suicide rates of 30 per 100 000 were registered among Brazilian Indigenous Peoples, and in Colombia it was calculated at 500 per 100 000, specifically for Embera People9,10.
The Ministry of Health and Social Protection of Colombia, with a participatory methodology, specified that suicide is a result of the frustration felt, especially by the youngest, because they cannot build their life project or because they do not follow the norms defined in the law of origin or because they have weaknesses in the ways of understanding and coping with the reality they live in9. This law of origin consists of what allows the original peoples to achieve cultural permanence; it is the principle of spiritual existence from which everything is legislated in harmony9.
Since 1970, a process of interdisciplinary collaboration has validated the biomedical, community and psychological approaches, leading to the emergence of a new intercultural psychiatry11,12. It has encouraged the establishment of policies for mental health; the integration of the treatment of neuropsychiatric disorders in primary care; the expansion of research in epidemiology, effects of violence, women’s mental health, mental health services and prevention; and strengthening of data tracking. These premises were supported by the design of research instruments that were cross-culturally validated13,14.
Lolas mentions that while the sciences progress, more is known about many ailments or better diagnostic and therapeutic resources15; however, these evidence-based practices are poorly implemented in many contexts. Research conducted in low- and middle-income countries has attributed the high rates of common mental disorders to factors such as discrimination, unemployment, and experiencing a period of rapid and unpredictable social change16, especially in young people. These causes will also be explained according to the concept of intersectionality, where rurality, youth, ethnicity and poverty are combined with mental illness to increase psychosocial risks17. In the case of Indigenous communities, the condition of rurality is especially added, since Indigenous communities inhabit, for the most part, areas that have small headwaters and low population density (<50 inhabitants/km2).
In the context of Colombia, a meaningful connection has been established between actions grounded in the developmental process and the Indigenous peoples and communities. This connection is supported by allopathic scientific evidence and is geared towards advancing mental wellbeing, nurturing spiritual and cognitive equilibrium, and fostering initiatives to prevent suicidal tendencies and the use of psychoactive substances. These efforts align with the broader framework of public mental health policies9,18.
Justification: Emberá Dobida case
According to the National Indigenous Organization of Colombia19, the Emberá Dobida Peoples are mainly grouped into two large blocks, one in the department of Córdoba and the other in the department of Chocó. Their ancestral origins trace back to a specific segment of the Emberá family, commonly known as the ‘chocoes’ linguistic group, and their current settlements are the product of all the pressure dynamics over their land and culture, which shows a close relationship with the territory.
In 2019, approximately 100 people from the Emberá Dobida Peoples, from Alto Baudó, began an exodus because of territorial problems. As is characteristic of this community, they were looking for a place to settle, near a river. However, multiple difficulties were presented in terms of territorial planning, land use permits, and health insurance. As they mention, they began to feel without a land.
Although not hallucinations as described in psychiatric semiology, noises were heard at night, some young people did not want to fish anymore, it was difficult for them to get up in the morning, they rejected the care of their parents, and they cried for hours. Given this situation, the leader of the settlement guided the young people, their mothers and their fathers to consult the nearest allopathic doctor. However, the health professionals did not find any indicator of mental problems or suffering, and the diagnosis was, in the words of the leaders of this community, ‘there is nothing, there is no illness’.
If an allopathic doctor is not able to find any problems, the young people and their families consult a ‘Jaibaná’ or traditional doctor. In his words: ‘When there is no disease of doctors, there is a spirit of death that must be fought’. In this case, young people and their families followed this process, but due to migration they did not have access to a Jaibaná, which implies for them ‘that evil has no solution, that there is no hope’.
Two weeks after the initial medical consultation, an epidemiological outbreak of suicidal behavior began, with a death by suicide of a person aged 16 years, who had also served as a translator of her assent. There was also a suicide of a girl aged 14 years, a sister of the adolescent mentioned above; a boy aged 16 years, an expert fisherman; a girl aged 15 years, also a new mother; and a person aged 18 years, an assistant in the local school. The events were all 1–2 weeks apart.
Many of the diagnosis of neuropsychiatric and behavior disorders are derived from precarious social conditions, such as poverty, hunger, violence, alcoholism, and abuse of psychoactive substances, that continue to exist in Indigenous communities in these conditions, which could be translated, from a broader critical view, as social or cultural suffering20. Despite clarity about these conceptualizations, very little research has been done in general health and much less in mental health in Indigenous communities21.
The conditions described above are identified as a priority public health problem, because apart from jeopardizing individual lives, in a great proportion in young people, they are a risk to the survival of these communities and merit future studies designed to approach the problem from an intercultural perspective. Livingston et al22 refer to the fact that the identification of risk factors for mental disorders is essential for the reduction of suicidal behavior, especially those related to parental practices. In addition, these instruments must have processes that are jointly created with Indigenous communities and sensitive adaptations to their contexts22-24.
Some instruments validated with non-Indigenous populations could allow some comparisons, but they fail to fully measure wellbeing and psychosocial risk variables24. Given the preceding context, the primary aim of this study was to undertake an intercultural construction process and validate an instrument. This instrument’s purpose is to identify challenges concerning parenting practices, emotions, behavior, and suicidal tendencies among Indigenous children and their families within community mental health services. Therefore, it was intended to design a scale for monitoring mental health problems in children and adolescents and parenting practices used in socialization from the perspective of caregivers, children and adolescents.
Methods
Design and procedure
A descriptive cross-sectional study was carried out to identify and describe the psychometric characteristics of the Parenting, Behavior, Emotions and Suicide risk scale (PACES) used to evaluate, (according to its acronym in Spanish), problems in parenting, behavior, emotions and risk of suicide, in community settings or in primary care mental health services at the first level of attention. This name also arises from the premise that mental health is a main tool in the construction of peace in the territories because paces in Spanish is the plural of the noun paz, which in English means peace. The leaders of the Indigenous Peoples of Colombia were invited to a meeting, and leaders and experts from the Emberá, Wayuu, Uwá and Awá Peoples participated.
At the meeting, the questions with the greatest weight of instruments validated in the Colombian population were selected. Among them were the Child Behavior Checklist (CBCL) 4-1825, the Parenting and Family Adjustment Scales (PAFAS)26 and the measurement of parental competence27. Of these instruments, the questions that the majority considered pertinent were selected and adapted, in addition to other questions related to the proposed domains. The CBCL27,28, the PAFAS29 and the parental competence instrument30 were selected for showing adaptation to the Latin American population and for having adequate sensitivity and specificity.
The consolidated instrument was presented to the experts to define the apparent validity31. Among these were a psychologist with a doctorate in public health, a psychologist with a master’s degree in clinical psychology, a social worker with a doctorate in family studies, an epidemiologist, a child and adolescent psychiatrist, a pediatrician with a master’s degree in children’s rights, and a clinical psychologist expert in psychometrics.
Through a form, each expert evaluated the items of the instrument. For the elaboration of the tool, 10 categories were considered on the items: clarity, objectivity, relevance, organization, sufficiency, adequacy, consistency, coherence, methodology, and significance. The V-Aiken (content validity) coefficient was applied to these items. Each one of the items was assigned one of the following categories: unnecessary, useful, or essential. In addition, it was inquired if each question was understandable, and modifications were allowed.
Instrument
After finalizing the ultimate instrument, it was applied in three Indigenous communities by health personnel with experience in intercultural mental health. Signed informed consent was obtained by participants. The PACES scale was made up of 42 questions in Spanish, and was divided into two sections: the first for main caregivers, and the second for children and young people 7–16 years of age. It had Likert-type response options – never (0), sometimes (1), often (2), always (3) – which indicated the frequency of presentation of the symptom or the difficulty.
The data were exported and analyzed by using the statistical program Statistical Package for Social Sciences v26 (IBM Corp.; https://www.ibm.com/products/spss-statistics). Univariate analyses were performed to determine measures of central tendency of the relative scores, and multivariate analyses were performed to analyze the degree of difficulty and discrimination. Internal consistency was also explored using Cronbach’s α coefficient for each of the scales; correlations were analyzed both within items and across scales to assess the degree of association and the extent of overlap between them; and the construct validity of the instrument was determined through factorial analysis.
With these results, a matrix was designed with values above the mean in each domain, and with the opinions of each professional to determine inter-rater concordance. This process is part of the validation of instruments, to verify reliability, to identify possible cases or to confirm the presence of a mental disorder. In order to perform the mentioned above, Cohen’s κ test was carried out32,33.
Participants
In this study, 168 caregivers of Indigenous children and adolescents, who responded to the PACES scale. participated. The instrument was completed by mothers, fathers, grandmothers, siblings and community educators (Table 1). The educational level was not queried because the instrument was administered with the healthcare personnel support, as it would be in primary care services.
The inclusion criteria were people 6–16 years of age, whose main caregivers agreed to participate in the study. In the same way, to participate in the study, the authorization of the leaders or governors of the Indigenous communities, the assent of the minors and the signing of the consent of the parents were required. Previous diagnoses of mental illness were considered as exclusion criteria. However, no participant had a previous diagnosis.
Ethics approval
This study was approved by the bioethics committee of the University of Manizales (CB-022), who validated compliance with the principles and ethical standards of the Declaration of Helsinki of 1975 and its subsequent revisions and also of Resolution 8430 of 1993 of the Ministry of Health of Colombia.
Table 1: Sociodemographic data
Results
According to the experts in intercultural mental health, all the items initially constructed with the towns and communities could be used in the scale. After applying the instrument validated by experts and making the minor modifications suggested by them, the scores across the domains were obtained as indicated in Table 2, specified by means and percentiles.
In this sense, above the 75th percentile, 40.47% were found in the case of parenting problems, 27.38% in perception of involvement, 31.54% in perception of bond, 31.54% in perception of monitoring, 27.97% in parental competence, 26.19% in self-perceived suicidal risk, 35.11% in suicidal risk perceived by parents, 25.59% in behavioral problems, 31.54% in emotional problems, and 34.52% in mental health risk.
The results of the t-test indicate that the items discriminated correctly and had an adequate level of difficulty, since statistical significance of p≤0.05 was obtained in all of them (Table 3).
The scale showed high reliability (α=0.911), while the independent assessment of each scale showed medium and high reliability values, as shown in Table 4. The values of the statistical estimation of the item-test relationship show that items 1.5 (‘Your child intentionally hurts himself’) and 1.7 (‘Your child does not obey at school’) did not meet the minimum values and puts in consideration their inclusion on the scale.
To determine the feasibility of performing a factor analysis, the Kaiser–Meyer–Olkin index was found for each of the scales, which should be greater than or equal to 0.5, and the Bartlett sphericity test, which should be significant (p<0.05). Subsequently, a varimax-type orthogonal rotation factor analysis was performed for each scale. For the choice of the items that make up each of the factors, the individual value of each factor greater than 1 and saturations for each item minimum of 0.30 were taken as criteria. Failing that, the highest factorial load was chosen, in case the item presented lower saturations than expected. The result of this analysis for each of the scales, parenting, behavior, emotions, and risk of suicide, is presented in Table 5. The questions that were eliminated in the factorial analysis received too a low score by experts in the initial panel, which suggests that the experts were knowledgeable about their respective communities.
Table 6 presents the correlations between the factors that make up the subscales of the instrument. Among the symptoms suggestive of seizures, there was an important correlation between the subscales of parental adjustment; bonding; monitoring; parental competence; self-perception of suicidal behavior; perception of suicidal behavior in caregivers; and affective, behavioral, and general risk symptoms in mental health. In the question that investigated the risk of hallucinations, a correlation was found with monitoring, self-perceived suicidal risk and behavioral symptoms.
On the other hand, among the subdomains there was a correlation of parental adjustment with the rest of the domains, as well as the perception of involvement, monitoring, and the affective bond, with parental involvement. Regarding parenting, a correlation was found between the domains of involvement (inquired of children and young people) and parental adjustment (inquired of the main caregivers). Behavioral and emotional symptoms, both asked of the main caregivers along with the perception of suicidal risk, also showed a significant correlation with each other, with the parenting domains and with the risk of mental health in general.
This is how the perception of suicidal behavior showed a significant correlation between the self-perception of children and young people, and the perception of their caregivers. Other correlations are specified in the mentioned table.
Regarding the concordance, carried out with 51 families that were assessed at the clinical level, between two evaluators and the results of each domain, an excellent concordance (0.81 and 1) is found in the Cohen’s κ measure for all domains, with the exception of parenting, which shows a good concordance (0.61–0.80)29.
Table 2: Descriptive statistics of the domains of the PACES scale (n=168)
Table 3: Analysis of the difficulty and the discrimination of the items of PACES based on the t-test
Table 4: Reliability analysis by subscales of the instrument
Table 5: Factor analysis of the PACES scale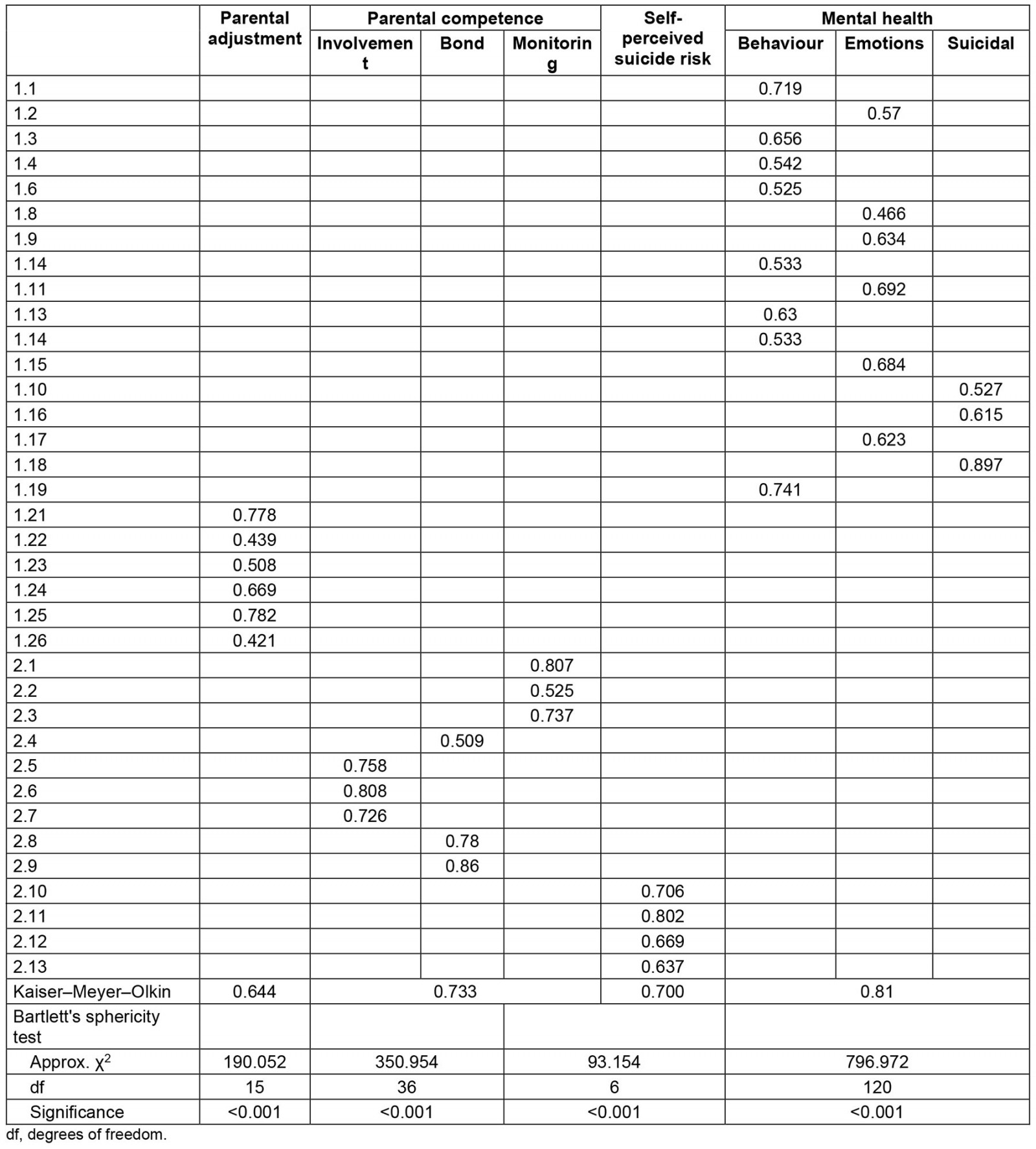
Table 6: Correlations and significance for PACES domains (n=168)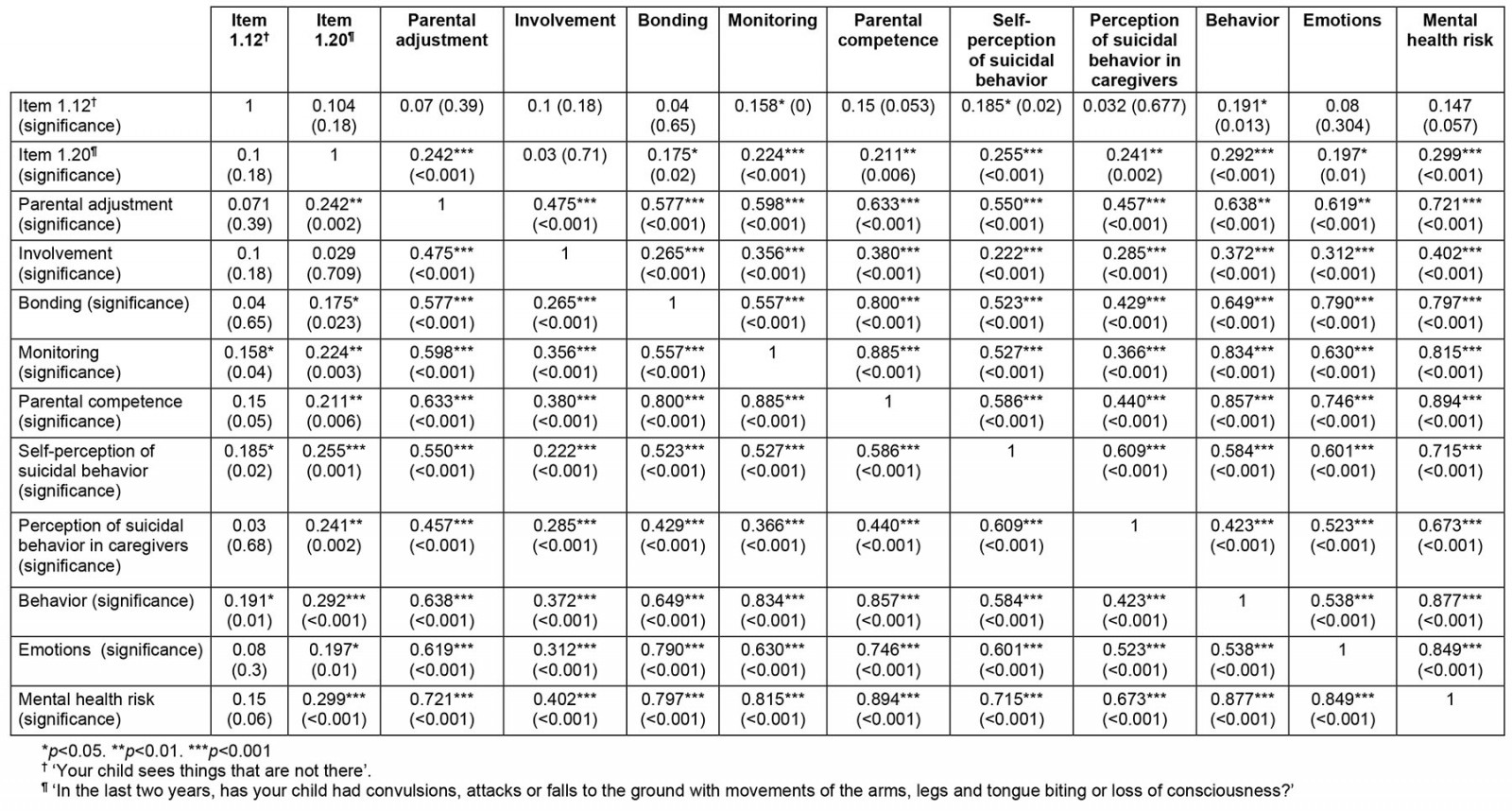
Discussion
The World Health Organization assigns an important responsibility for the wellbeing of children and adolescents, to the first level of care and to community settings, with the active participation of the communities themselves in care34. The objective of this study was to carry out a process of participatory construction and intercultural validation of an instrument to determine mental health risks in children and young people in indigenous communities (see Appendix I). Adequate psychometric properties were found in the instrument, where there was coincidence between the reports given by parents and good parental experiences in the population of children and adolescents.
Other studies have pointed out the importance of directly considering children and adolescents in the instruments, in addition to contrasting with information from caregivers and health personnel themselves35. Like the Aboriginal Children's Health and Well-being Measure developed for children and young people (8–18 years), and the Session Rating Scale that includes four strengths-based questions related to relationships, goals, themes, and overall rating, the tool designed includes measures of positive wellbeing based on children’s and other community members’ understanding and perspectives on wellbeing8,35,36.
PACES presents as a strength because it follows some guidelines proposed for the development of measurement instruments in Indigenous Peoples8: it is carried out to detect early alterations in the perception of wellbeing, it incorporates questions related to affective ties and relationships, it has a component of self-administration and another one of administration by caregivers, it has adequate reliability and validity, and it can determine risk levels8,37.
Through the PACES scale, it is intended to address, in the same instrument, variables related to pediatric mental health from the perception of the caregiver and from the perception of the child or adolescent, in addition to including relational variables in the same questionnaire. This is consistent with the worldview of Indigenous groups, who believe that parenting practices are closely related to cultural connection and wellbeing38.
The preliminary results of PACES confirmed that having good mental health for Colombian Indigenous Peoples implies a concept of comprehensive health that is comparable to that of good living, without distinctions between physical and mental health; therefore, the promotion of culture among young people, and the active participation in traditional practices and subsistence activities and in community life protect Indigenous mental health1.
Among the Emberá People, a continuous connection with their territory is evident, as they consistently uphold practices encompassing control, security, healing, punishment, protection and oversight. For an Emberá to be protected by the spirits, they must belong to the territory, because this way, it protects them from evil spirits and malicious jaibanás39. One potential limitation of this study arises from the absence of domains closely linked to Indigenous mental health, including issues such as violence, displacement, nutrition and acculturation8,22.
Another limitation is related to the sample size. Although the Indigenous population is less than 5% of the total Colombian population, this study was conducted with a sample of only two out of more than 80 indigenous communities that live in the country. Therefore, future research should include more communities to obtain adequate validation information for each community and increase the representation of Indigenous beliefs about mental health and wellbeing.
However, beyond translating the instrument to each community, the forms of individual, family and collective health care of each Indigenous Peoples in the territory must be known; the social, environmental (territorial), spiritual and thought conditions that produce own and non-own disharmony must be known; and the factors of disharmony must be identified, within the framework of their own medicine, for each moment of life (as defined by each people) and the necessary intercultural and individual actions to restore balance40,41.
Conclusion
It is important to remember that the vulnerability of Indigenous Peoples is based on how political, economic, and cultural structures give rise to mental health problems and how these intersect in particular ways that are harmful to these people. Therefore, PACES should be considered as a tool, which means using it not just to detect problems in the Western tradition but to approach primary care in line with the well-living expectations of Indigenous Peoples. So, any mental health program for Indigenous Peoples must offer a psychology and psychiatry community perspective broad enough to address the needs of both individuals and the local worlds in which they live.
Finally, as recommendations for subsequent validations that accompany this instrument, it is necessary that health systems provide relationship spaces for intercultural dialogue that is essential for understanding these problems and disorders from the Western health system and Indigenous cosmovision (collective and individual worldviews), and the spaces and times that the Indigenous Peoples and the institutional framework agree to respect and make flexible in the cases that are required for access to territory, climatic condition, and prior harmonization, among others. Also, it is recommended to have an Indigenous translator (bilingual guide) who can support communication at the time of the consultation. Most of the Indigenous Peoples who have their own language can talk about their situations more freely when they can talk in their language.
Acknowledgements
The authors thank Nancy Millán Echevarría and the Original Peoples of Colombia.
Funding
This study did not receive any funding.
Conflict of interest
The authors declare no conflicts of interest for this research.





