Introduction
In its most recent report on the nursing workforce, the WHO estimated that an additional nine million nurses and midwives will be needed by 2030 to meet global healthcare needs1. As a professional group, nurses represent almost half of the worldwide health workforce and play a critical role in providing health care, from tertiary through to primary and community-based settings2. The lack of an adequately sized nursing workforce thus has fundamental consequences for the accessibility and quality of health care provided to communities1,2. It also detrimentally affects the health and wellbeing of the existing nursing workforce and damages community perceptions of health services, further exacerbating attrition, and the acceptability and utilisation of health services1,3.
In the rural health workforce, which in this context refers to practitioners practising outside of metropolitan and regional centres, nurses are described as the backbone of the healthcare system and may be the only health professionals from whom care and treatment can be received4-9. This is certainly the case in remote and isolated locations in Australia. In these locations, nurses constitute the single largest cohort of healthcare professionals4-9 and provide care models for local residents to address a range of health issues across the lifecourse10. The current global nursing workforce shortage, driven by a decline in enrolments and at the same time as increasing demand from an ageing population1,11, has significant and far-ranging implications for rural, remote and isolated communities. This is in the context of enduring issues for rural, remote and isolated places, with workforce maldistribution caused by workforce shortages and high staff turnover contributing to health disparities12.
Many of the factors contributing to attrition and turnover within the nursing workforce – the decision to leave a position13,14 – are relevant to all practice contexts. However, rural and remote nursing is widely recognised as a complex and unique profession with a broad scope of practice7,9,15-19. Further, there are increased rates of burnout in these locations compared to larger regional or metropolitan centres. The higher numbers of fly-in fly-out (FIFO) workers in these contexts can contribute to this issue given that the work of orientating and training FIFO workers, who routinely rotate through different places, is often assigned to the few permanent in-place staff8,12,15,20-22. Consequently, some issues pertaining to the attraction and retention of nurses in rural, remote and isolated practice contexts are unique4,5,9,20,23-26. In Australia, governments have invested in developing strategies aimed at strengthening the rural and remote nursing workforce19,27-35, which have made some, though not substantial, progress4,5. A key gap in current understanding and strategic action is the limited investigation into what nurses currently practising in rural, remote and isolated locations view as important for improving the attraction and retention of their workforce and reducing avoidable resignation (also referred to as avoidable turnover, turnover intention and decision to leave)14. These perspectives are vital to informing the development of an integrated person-centred and whole-of-lifecycle approach to improving the attraction and retention of the rural and remote nursing workforce.
The purpose of this article is to present an analysis of existing literature that reports rural and remote nurses’ views on what informs the attraction, retention and resignation of this workforce. This includes examining how the motivations and values underpinning the views and experiences of nurses in rural, remote and isolated settings have been considered in the field to date. In doing so, we hope to provide researchers, rural and remote health service managers and policymakers with useful guidance on future actions that respond to the issues identified by nurses in these contexts.
Methods
A structured scoping review was undertaken to identify current knowledge, from a nursing perspective, about the attraction, retention and resignation decisions of nurses in the rural and remote workforce in Australia and explore gaps in the available literature. The review process was informed by Arksey and O’Malley’s framework for conducting scoping studies36, which specifies five stages that enable a consistent approach, from formulating an appropriate question to summarising and reporting findings. In addition to Arksey and O’Malley’s scoping studies framework36, discrete chapters from Boland, Cherry and Dickson’s text on undertaking systematic reviews and Liamputtong’s work on research methods and evidence-based practice informed the approach taken to the organisation and synthesis of data and the review of qualitative evidence37-41. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis Extension for Scoping Reviews (PRISMA-ScR) checklist was also used to guide the reporting in this review42.
Identifying the research question
The initial research question guiding this review was informed by the first author’s prior knowledge and experience as a practising remote area nurse (predominantly within the state of Queensland) and conversations with other nurses in the remote workforce. Some preliminary literature scans were conducted in April 2022 to gain a sense of current scholarship and assess the availability of sources to address this area of inquiry. These initial literature scans identified a need for a greater understanding of attraction, retention and resignation within the remote nursing workforce from the perspectives of nurses practising in these contexts. Drawing on this indicative search of extant literature, the research question guiding the current review was refined to ‘What are the perceptions, values and motivations of nurses practising in rural, remote and isolated settings of Australia about attraction, retention and resignation within their own workforce?’ The decision was made to include rural as well as remote and isolated settings to account for particularities and similarities between these practice environments and ensure potentially pertinent literature was not overlooked.
Identifying relevant studies
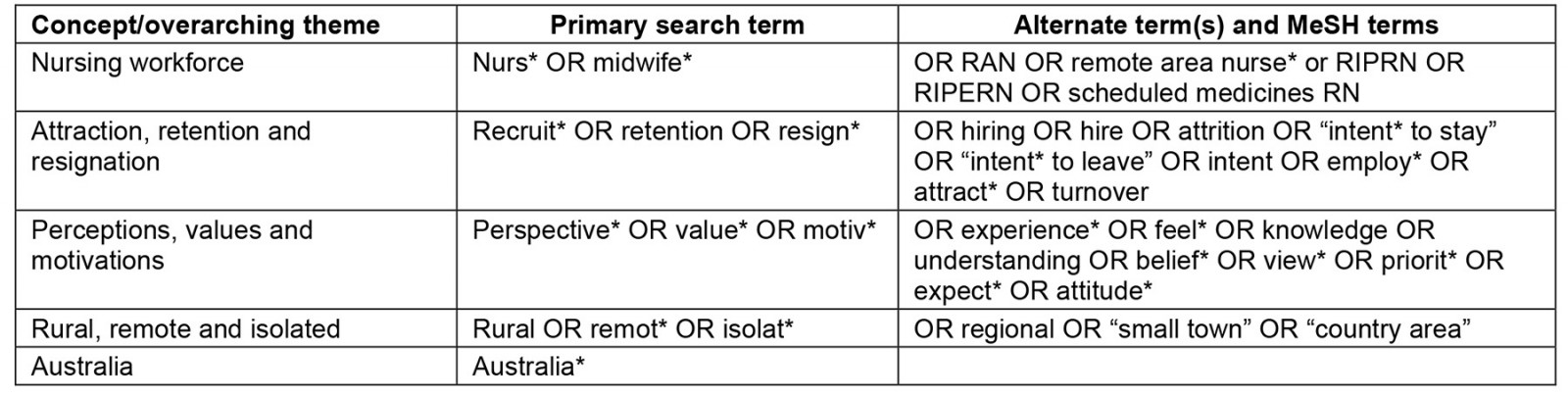
A comprehensive list of search terms (Appendix I) was generated to identify relevant studies, informed by the preliminary literature scans referenced earlier. A series of inclusive search strings (Table 1) was then developed and trialled from these terms, with the assistance of a highly experienced specialist librarian, whose advice was also sought to select appropriate databases to search. Here, consideration was given to the nature of the content expected and the reputation as relevant and reliable databases. Six databases were selected: CINAHL, PubMed, Embase, Medline, Scopus and Cochrane Library. Each database was then searched in August 2022 using the refined search strings, adjusted to account for database-specific variations.
Study selection
The searches deployed across the selected databases yielded 714 results. Given the similarity and number of search results between PubMed and Medline, the results from Medline were excluded. Results from the Cochrane Library were also excluded, as none were relevant to nurses’ perspectives, values or motivations. Results were scanned for duplication, and all duplicates were removed (n=421). The titles and abstracts of all other identified studies were then screened by the first author using predetermined inclusion and exclusion criteria (specified in Table 1). Here, it is emphasised that only studies detailing the values, perceptions and motivations of nurses practising in rural, remote or isolated locations, based on data collected directly from nurses working in these contexts, were included. Where the first author could not make a clear include/exclude decision, the second author independently reviewed the title and abstract to make this decision, which was discussed and confirmed with the first author. When neither the first nor second author could make a definitive decision, the third author also reviewed and a decision was made through discussion. Following this process, the full texts of all remaining studies (n=50) were reviewed to confirm the final selection of included studies, of which there were 12. Figure 1 outlines the number of articles reviewed and excluded at different stages in the process. Throughout this screening and subsequent stages of the review, the research question was revisited by all authors, who worked collaboratively to ensure decisions were made with reference to this question.
Table 1: Study inclusion and exclusion criteria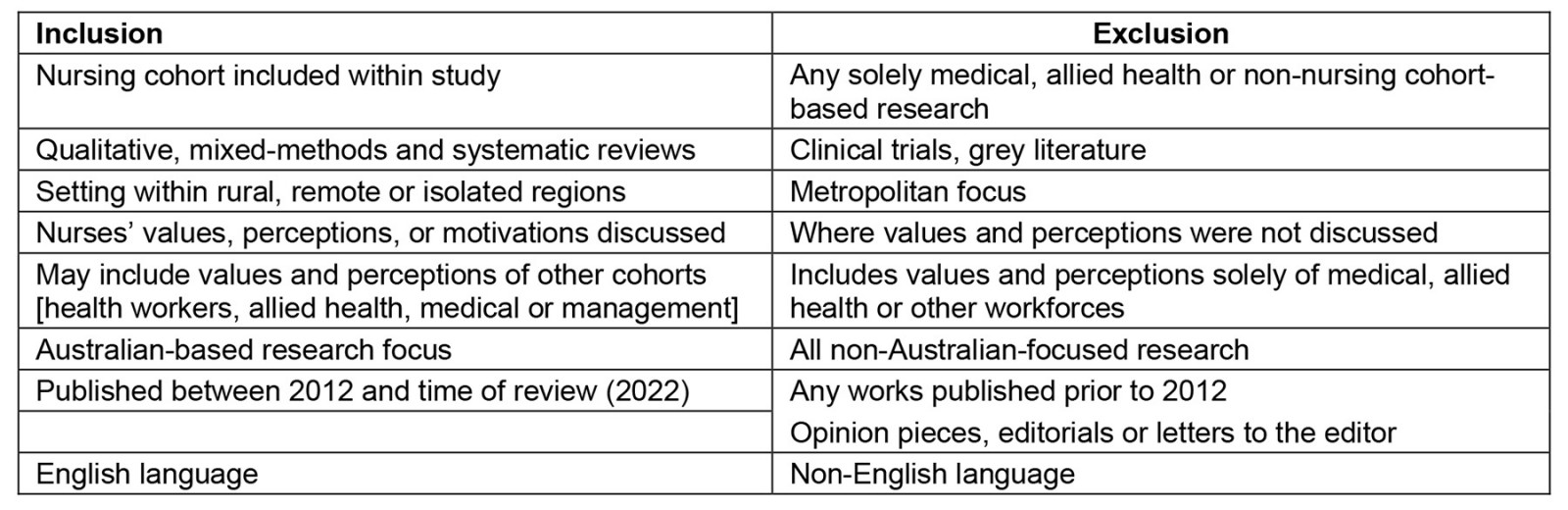
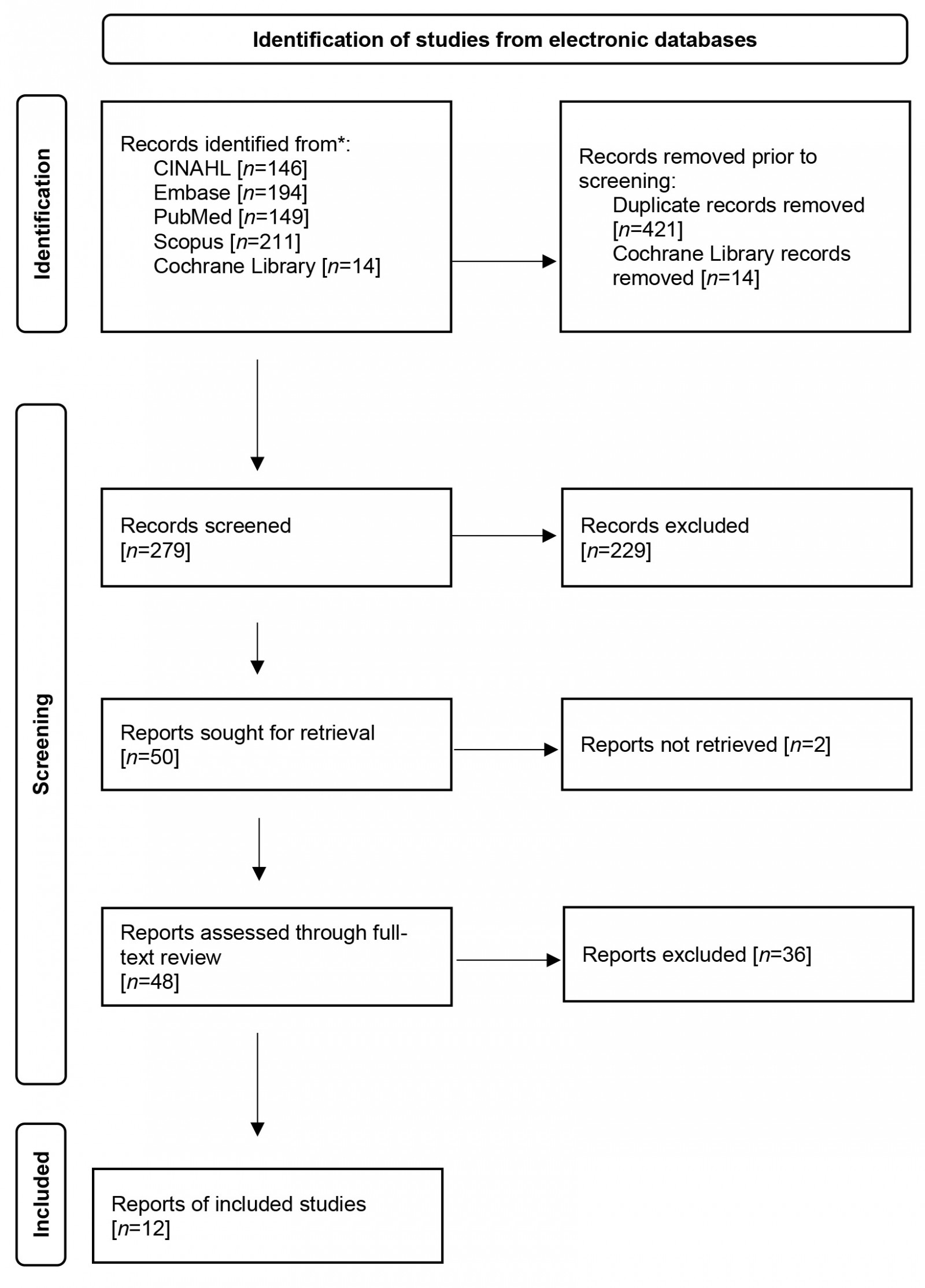 Figure 1: PRISMA 2020 flow diagram.
Figure 1: PRISMA 2020 flow diagram.
Charting the data
The key methodological details, including the setting or location of the research, its aim, methods employed and sample, were extracted and charted along with findings pertinent to the research question guiding the review from each included article (Table 2). This provided a contextualising and accessible summary of the reviewed research. From this foundational synthesis, a deeper analysis was built.
Table 2: Methodological details and relevant findings in reviewed literature14,43-53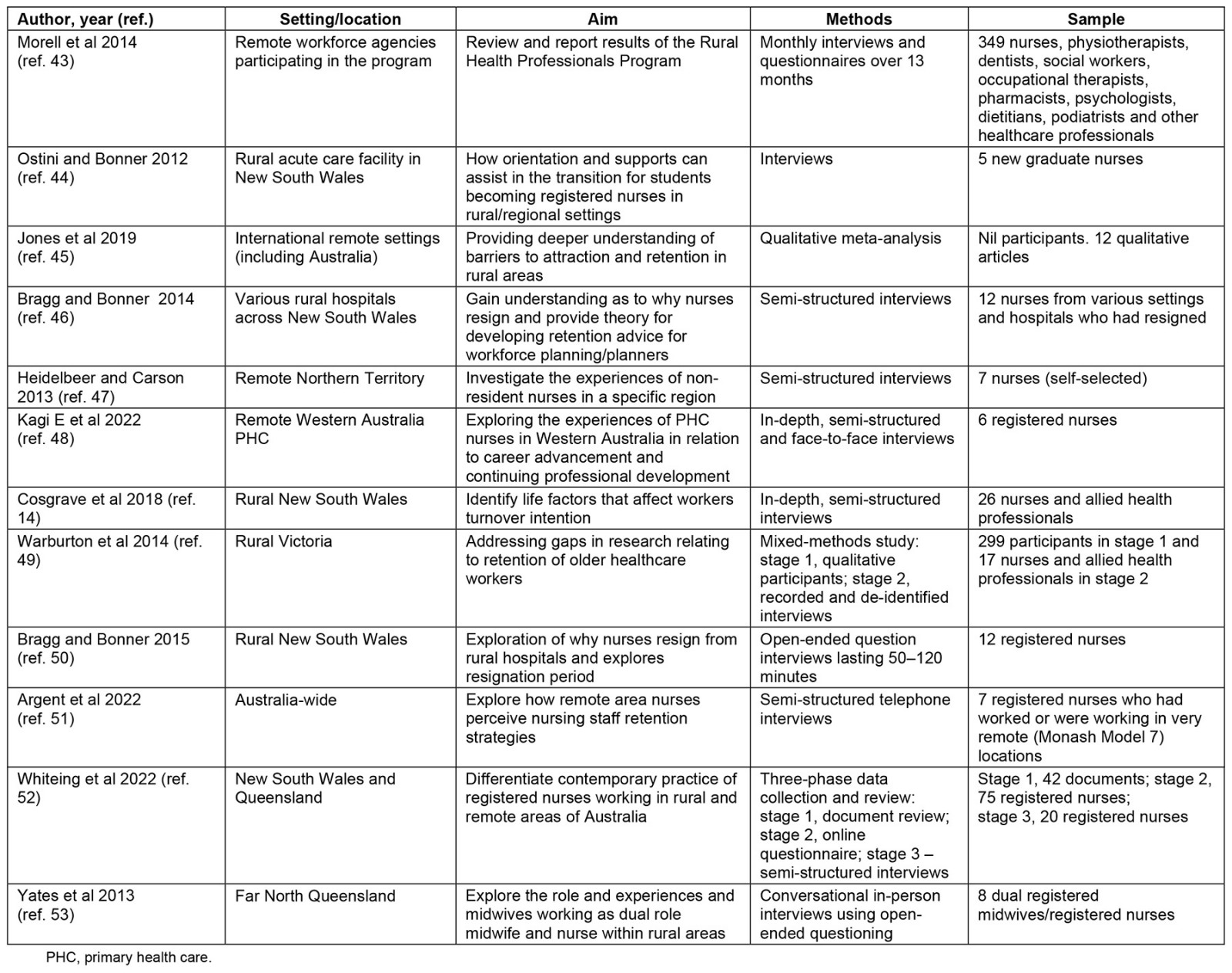
Collating, summarising and reporting the results
Cosgrave’s person-centred retention improvement framework12, which includes attraction and recruitment, for addressing health workforce challenges in rural contexts, was used to aid in synthesising and interpreting information from the included studies. This framework provided a clear structure in which the specific themes related to attraction, retention and resignation that were identified in the included studies could be located and considered. It also enabled the interconnected nature of the issues articulated in these themes to be conceptualised in a nuanced manner. Information from the studies pertinent to each of Cosgrave’s domains12 was analysed and collated thematically, first reviewing the studies and then creating appropriate codes relevant to each54. Candidate themes were then refined to elucidate issues specific to different lifecycle stages. The identified themes are mapped to the lifecycle stages of attraction–retention–resignation in Table 3.
Table 3: Themes relevant to the three lifecycle stages14,43-53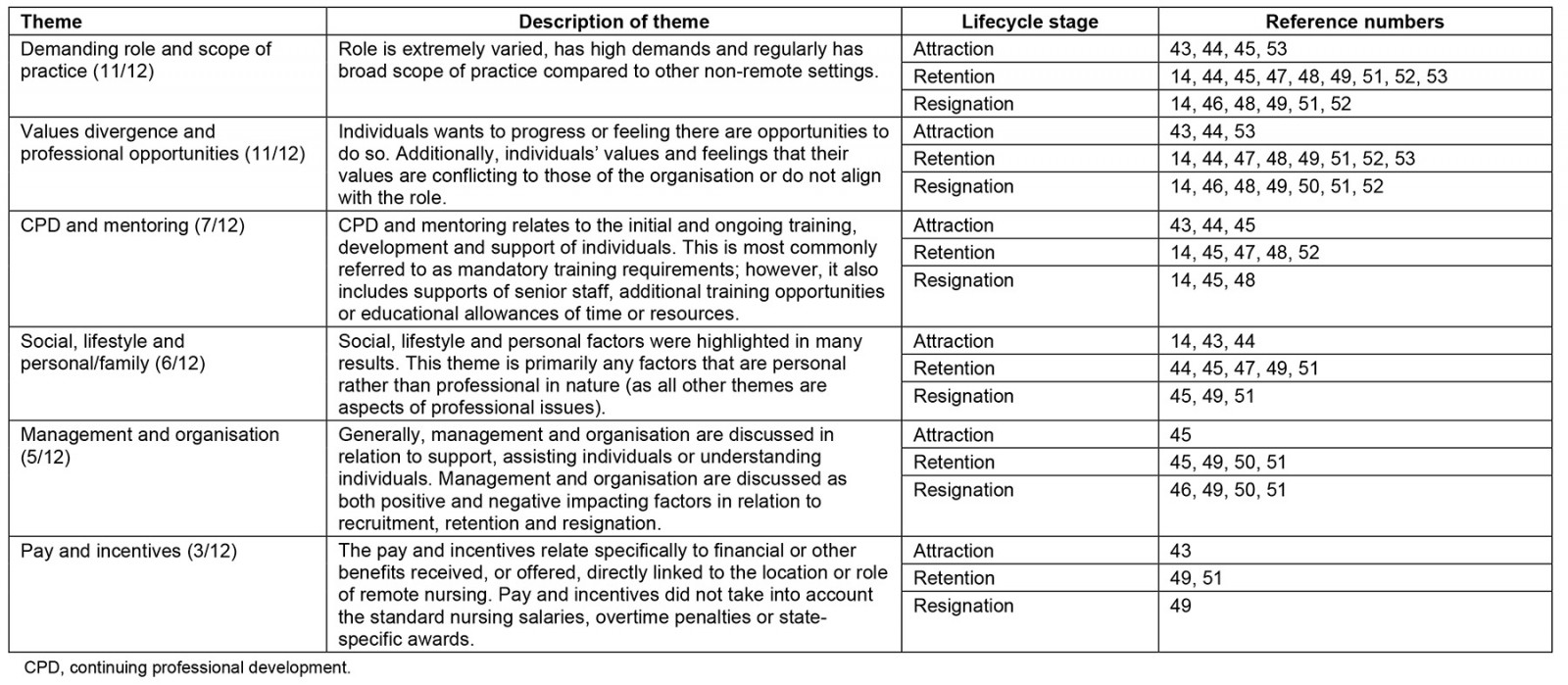
Ethics approval
This scoping review used only peer-reviewed, published data, so it did not require ethics review or approval.
Results
Twelve articles met the inclusion criteria of this review; Table 2 provides a summary of each article. A range of research methodologies, including qualitative, scoping and other reviews, as well as mixed-methods, were utilised in these included articles, which provided different forms of evidence and insight into nurses’ perceptions, values and motivations pertaining to the attraction, retention and resignation of their workforce. Six themes were identified and labelled:
- demanding role and scope of practice
- values divergence and professional opportunities
- continuing professional development (CPD) and mentoring
- social, lifestyle and personal/family
- management and organisation
- pay and incentives.
The findings of each of the included articles contributed to the development of these six themes (Table 3), which provides confidence in the interpretation of sources55. These six identified themes were then conceptualised within Cosgrave’s framework12 and the overarching lifecycle stages of attraction, retention and resignation. The complex way these themes overlap and interconnect is discussed below. The numbers presented in brackets after the name of each theme indicate the number of articles in which the specified theme was identified.
Demanding role and scope of practice (11/12)
The roles’ demands, pressures and uniqueness were described as factors that either drew nurses to rural, remote or isolated settings or led them to leave these practice environments14,43,45,47-49,52. Nurses who reported being drawn to and remaining in rural, remote or isolated settings tended to discuss the overwhelming professional satisfaction derived from their work. While this led to retention in the medium term, it was also described as a complicating factor for many when the decision was made to leave; these nurses reported a sense of failure if the role became too much or other circumstances required them to move away52,53.
Relatedly, the scope of practice was specifically identified as a factor informing intent to stay. Nurses reported experiencing tension when the scope of practice, expectations of colleagues or superiors, or safety concerns did not align with their professional values or understood boundaries within their roles44,46-48,52. Unclear job description(s) or scope of practice was viewed as a barrier to attraction and a tension for retention. As explained in more detail in the final theme presented, the scope of practice and delineation of roles were also linked to pay and incentives in relation to retention or resignation47,48.
Burnout, characterised by ‘emotional exhaustion, depersonalisation, cynicism, detachment and a low sense of personal accomplishment’56, was regularly discussed by nurses in the context of the demands of the role. To manage burnout specifically, it was reported that some rural and remote health services put in place flexible work arrangements, or individuals undertook the work as full-time or contractor staff that allowed time to relieve related work stressors49,51,53. One such example was individuals working for 3–6 weeks before taking time off or travelling back to their home location54. However, in these cases it was noted that flexible arrangements were often insufficient to reduce burnout or were not implemented in partnership with the nurses involved47,49. Therefore, it was unsurprising that all participants in one article listed workload pressures as the reason to either consider or follow through with resignation49. These workload pressures ranged from feeling that shift and on-call requirements were no longer manageable to being ill-equipped or underprepared for the role, the expectations of patients, community or higher management, or being overwhelmed or burnt out from the work49.
Values divergence and professional opportunities (11/12)
Professional opportunities in rural, remote and isolated environments, which were frequently tied to the notion of professional pride, were identified as important factors for attraction and retention14,43,44,47-53. Many available nursing positions in the rural and remote workforce allow for speedy advancement as a junior clinician. Variation of positions and opportunity to undertake ‘multi-hatted’ roles that would not be considered standard practice in metropolitan settings are more likely in rural, remote or isolated practice settings. These opportunities for advancement and role experience were highly valued, especially among junior to mid-career nurses, and were a motivating factor in choosing a rural, remote or isolated practice environment over metropolitan or larger regional contexts43,44,47,48,51,53. In contrast, nurses who had either practised for some time or previously occupied senior roles expressed frustration and disillusionment with the lack of career progression past a certain point in these practice environments and experienced great difficulty with professional isolation14,46-50,53. This led to a sense of disconnection from their wider nursing cohort, and motivations to stay in the role diminished over time.
Several of the included articles explored the concept of value divergence, where an individual’s professional values do not align with hospital values14,46,47,49. In such circumstances, nurses reported feeling unable to perform their roles safely, and pressured to perform uncomfortable tasks that were pushing the legal boundaries of the scope of practice – a combination of training, education, legal authority and individual skill level. Specific examples of value divergence reported in the included articles were finances being more important than patient care, timeframes placed on care in lieu of comprehensive or quality care and attention, or pressure to perform patient care in a way that was compromising46. These experiences and the broader theme to which they have been assigned here link to the theme of scope of practice discussed earlier and to effective workplace supports.
Continuing professional development and mentoring (7/12)
The importance placed on CPD and mentoring in the context of attraction, retention or resignation was significant in seven of the included studies14,43-45,47,48,52. Training provisions were regularly highlighted as a significant driving factor for nurses when seeking out or continuing in a rural or remote role14,44,45. When nurses perceived that there were opportunities for professional development, training and growth, it most often had a positive impact on attraction to and retention in a rural or remote role43-45,48. Conversely, there was a strong link between resignation or intent to leave and a lack of support for CPD, which included the expectation that nurses needed to make their own arrangements for training outside of an already-demanding role45.
Many nurses in the included studies explained that there were times when even mandatory training, such as yearly clinical competency training – required by their employer – could not be attended due to work demands, had to be done in nurses’ own time, or was paid directly out of nurses’ own pockets to enable attendance at courses provided externally because it was the only way participation in the training could be facilitated in a timely manner45,47,48. In interview studies, nurses clearly articulated how the difficulties involved in undertaking CPD caused exhaustion and made them feel degraded and, ultimately, unsupported in their roles. This theme strongly correlated with that of management and organisation – discussed below – with many nurses expressing that, while their management was largely approachable when it came to needing support or resourcing for CPD and training, there was little to no input or backing14,45,48. In this context, nurses highlighted the importance of managerial and organisational support of CPD, both for the value of training itself and as a clear illustration to nurse employees that they are valued.
The concept of mentoring was closely linked to professional development in terms of organisational and management support. This included individual development, organisational facilitation of training, senior clinical mentoring and physical training43-45,48,52. Nurses in the included studies discussed the importance of having a ‘buddy’ system in the early stages of working in rural, remote or isolated settings. They suggested that retention would improve if ongoing mentoring, peer supports and professional mentors were facilitated or encouraged by organisations and management44,48,52. One of the included articles focused specifically on the experiences of new graduate nurses and found that junior clinicians were highly impacted, positively and negatively, by their experiences with senior support staff, clinical training, professional development, advancement opportunities and mentoring partnerships44. Participants in this study represented a good cross-section of junior clinicians in similar circumstances. The impact on attraction, retention and resignation highlighted, in this instance, that those who felt unsupported were more likely to have intentions of leaving, while those with positive experiences of mentoring and support for CPD intended to stay.
Social, lifestyle and personal/family (6/12)
Many nurses and healthcare professionals view rural, remote or isolated work in a romanticised and idyllic light, and some nurses consider moving to these areas for such reasons44,45,49,51. While lifestyle, social, family or personal factors did not appear to be the sole reason for deciding to stay in or leave a rural or remote position, nurses in the included studies were often motivated by such factors. Along with organisational ‘fit’ and a desire for professional development, nurses in the included studies regularly referenced a sense of belonging to place, personal and cultural exploration, cultural understanding, socialisation, or travel and adventure as important considerations for working in a rural, remote or isolated setting43,45,47. In some of the included articles, lifestyle and personal factors, including lack of supports, services, or activities for families, featured in nurses’ decisions about where to practice across the lifecycle45,47. Alternatively, there was a common sense that working in small communities demands a constant work persona, which leaves little time to rest and reset between shifts or to socialise with other community members as friends rather than patients45,49.
In considering lifestyle, nurses in the included studies often raised family and social factors as the main drivers for considering a position in rural, remote or isolated locations. For example, some nurses considered a FIFO role preferable for lifestyle as they could be fully ‘at work’ while remote and fully present at home outside of work47,49. Others, however, discussed the difficulties of being away from home for extended periods while working as a FIFO nurse, including missing special occasions or having a messy or unpredictable routine49,51. Here, it was expressed that they could not truly have the remote lifestyle unless living in the area, but the toll this lifestyle can take on family and other relationships was described51. Both permanent and FIFO nurses noted that the opportunity to be in and engage with many rural, remote or isolated communities was a positive and unique benefit to the work; in some instances, there would be no other opportunity to gain familiarity with certain communities and places47,49,51. Given the distance to previous home location, immediate or extended family, general geographic isolation and complications these issues cause to personal lives, many nurses reported not having the ongoing motivation to remain in rural, remote or isolated settings, even when they were professionally satisfied49,51.
Management and organisation (5/12)
Although not unique to nursing or to rural, remote and isolated settings, the impact of management and organisational factors on staff attraction, retention and resignation rates was raised in several of the included articles20,25,27,32,45,46,49-51,57,58. Feeling valued and supported by management and the organisation was identified as important to the professional satisfaction of many nurses in the included studies45,46,49,50. This theme was found to resonate strongly in the retention and resignation stages of the lifecycle45,49,50,52.
Nurses who felt valued had a greater propensity to take a role or entertain a position in a rural, remote or isolated place45. Similarly, some nurses in the included studies explained that their resignation, or intent to resign, was a direct result of management or perceived lack of organisational valuing45,46,49-51. These studies highlight how both retention and resignation intent are strongly linked to and impacted by management style, leadership and how organisations value (or not) their nursing staff. When considering if they would stay in a role, nurses in the included studies cited perceptions of how they were valued within their organisation’s multiple times46,49-51. For instance, nurses who felt that an organisation valued their experience and backed them in all circumstances were more likely to remain in their position longer49-51. The opposite was also true: when nurses felt that their organisation was not supporting them, or that their values were compromised or no longer in alignment with those of the organisation, there was no other option but to leave the role, despite having a desire to stay for their patients or the community50.
Pay and incentives (3/12)
Pay and incentives were cited as factors impacting nurses’ motivations for taking up rural or remote positions. However, it was the least prevalent and expanded-upon theme identified across the included studies43,49,51. Overarchingly, discussions pertaining to pay and incentives related to how individual nurses understand remote work as more highly remunerated than metropolitan-based work43. Yet nurses in the included studies who had been working in rural, remote or isolated places for a longer period did not always consider the higher wage adequate, given the level of responsibility within the role49. For example, in two of the included studies, nurses who expressed feeling their organisations did not value them in the remote setting specified that this was, in part, illustrated by inappropriate compensation, incentive packages, monetary supports and a lack of other benefits49,51. For these nurses, the ongoing experience and skill of remote nurses are not systemically recognised.
One study discussed a program designed to recruit nursing, dental and allied health professionals into rural and remote work43. One of the factors specified as impacting the decisions of health professionals in this study was that of pay and incentives: this was listed as one of the primary factors for participants (including nurses) considering involvement in the program, with 51% of participants identifying this as their reason for participation43. In another article, the importance of financial stability and preparing for retirement in the stay/go decisions of nurses was highlighted, although not discussed or explored in detail49.
Discussion
This review provides a comprehensive overview, from an Australian perspective, of what underpins the attraction, retention and resignation of nurses in rural, remote and isolated settings from the perspectives of nurses practising in these environments. In undertaking this review, several clear gaps in existing literature were identified. For example, limited empirical research has adopted a whole-of-person combined with whole-of-lifecycle approach to understanding the rural and remote nursing workforce; the evidence produced through such approaches is required to appropriately plan for and target solutions for the future nursing workforce. This is especially the case in the context of ongoing and chronic nursing shortages, which are also occurring internationally. The lack of such research in the present context indicates that translational research on the nursing workforce that explicitly includes and engages with nurses is fundamentally needed. The implications of this review’s findings for rural and remote workforce development, health service and policy planning – issues of key concern for health departments globally – warrant further investigation to allow nurses to provide high-level care in a supportive environment with appropriate personnel on the ground.
In contrast to equivalent metropolitan-based nursing positions, for which there are most often clear role descriptions, supports, pathways and training programs, this review underscored a lack of understanding at a broader level around available supports, transition programs, the scope of practice boundaries, or personal capability required in rural or remote positions. In considering the matter of attraction, this review’s findings emphasise the importance of:
- exposure to rural, remote and isolated places as part of undergraduate and post-graduate training26,28,34,59-61
- clear scope of roles and expectations for rural and remote-based roles16,34,47,52,62
- pre-requisite pre-commencement training, including remote specialisation, cultural and local area awareness and scope of practice familiarisation26,47,52
- training and development of local rural and remote nurses to work in their own communities (including Indigenous programs)19,34,62.
These four strategies would better enable the attraction of nurses who are a good fit for the role, enhance intent to stay longer term, and improve the overall stability of the health workforce in rural, remote and isolated communities. Given that attracting a rural health workforce is a global challenge62, there is merit in exploring the applicability of these strategies in other international contexts.
While not easily decoupled from attraction, most of the included studies focused on factors affecting retention. In considering the findings of this review through a retention lens, several short- and long-term strategies deployed at the organisational level can be recommended, which again are likely to have relevance to other rural places in the world where the retention of nursing staff is a challenge. In the short term, these include instigating a systematic process of proactively seeking feedback from nurses throughout their tenure50,57 and providing nurses with a clear and accessible path to discuss concerns with management or key organisational leads. For long-term impact, eight strategic actions can be recommended based on the findings of this review:
- Introduce (or improve) hospital and health service induction and social orientation packages into the organisation and the community for new-to-place staff63.
- Introduce skill- and experience-based pay and incentives to link incentives to longer-term contracts and role demands20,22,64-67.
- Develop a rural and remote nursing progression program to cultivate and enable professional growth across the full career span.
- Introduce additional supports for CPD beyond mandatory training and leave types associated with participation in this training18.
- Develop relevant training packages, co-designed with nurses, based on local and individual needs9,16.
- Implement strict fatigue management and leave protocols to reduce burnout and intent to leave (ie no on-call past a set number of hours, and leave must be taken every set number of days/months).
- Develop a systems-supported mechanism for finding appropriate replacement staff for leave periods to lessen the pressure on rural and remote nurses to return to work hurriedly19,20,68.
- Establish a well-planned mentoring and peer support program for new and experienced rural and remote nurses (buddying up new arrivals with experienced team members) to ensure that nurses across the career spectrum have colleagues to bounce ideas off and feel heard and supported in their roles.
Improving the attraction and retention of nurses in rural, remote and isolated practice environments will reduce the need to focus on resignation within this workforce. However, this review’s findings suggest several actions that could be taken at an organisational level to ensure continued improvement and future support to the nursing pipeline. This includes the following actions:
- Establish a process for capturing data on staff’s job and personal satisfaction before resignation to better enable proactive actions69.
- Instigate routine exit interviews with resigning nursing staff to examine reasons for resignation, experiences of the organisation, and suggestions for improvement with clear systems for this de-identified data to be reported in thematic form to line managers and executive staff50.
- Review of vacant position scope of practice, role descriptions and needs of health services for appropriate nurses for the incoming position, applying a person-fit-environment recruitment process to support recruiting suitable candidates for job and community12.
- Develop a process for providing exiting staff with the opportunity to use their skills and experience to support future staff (ie mentoring, training, teaching or peer support)15,68.
Limitations
This scoping review intentionally focused on Australian studies, which, while putting a constraint on the results, enabled a specific, place-conscious research aim to be addressed. In acknowledging this place focus, it is also important to highlight that, increasingly, stronger similarities in context and experience are being found between rural places in different parts of the world than between rural places and metropolitan centres within the same national boundaries70. This suggests the review’s findings have value and relevance beyond Australia.
The review was limited to the views of nurses rather than health professionals more broadly or community members and other key stakeholders. It was also outside the scope of this review to explore how the specific issues pertaining to attraction, retention and resignation identified by nursing staff impact patient outcomes, health service demands or patient satisfaction, but this is valuable research to pursue in future work. Lastly, the scoping review methodology does not incorporate an evaluation of the quality, scope or level of evidence in included studies. However, opinion or editorial pieces were excluded from this review.
Conclusion
This scoping review provides insights into the perspectives and concerns of nurses practising in rural, remote and isolated settings in Australia, focusing on issues affecting their workforce based on 10 years of past research. The results of this review suggest that there would be significant advantages to a considered, holistic, lifecycle-stage-focused approach to attraction, retention and resignation within the rural and remote nursing workforce. This will likely continue to be a key topic of discussion in the context of overall nursing workforce shortages and the considerably unique position and scope of available remote and isolated work in particular. This review also found that comparably little region-specific research has been undertaken on this topic, which suggests further research in this area with the potential for broader application is needed.
Acknowledgements
The authors would like to acknowledge and thank Mr Cameron Rutter for his expert guidance on the search strategy and Dr Catherine Cosgrave for her critical feedback on an earlier version of the manuscript.
References
You might also be interested in:
2004 - Oil doom and AIDS boom in the Niger Delta Region of Nigeria